Table of Contents
Understanding Ketamine Infusion Therapy
Mental health challenges like persistent depression and anxiety affect millions, often leaving individuals feeling trapped despite traditional treatments. In recent years, ketamine infusion therapy has emerged as a promising, rapid-acting option for those seeking relief from treatment-resistant conditions. This innovative approach offers hope where conventional antidepressants fall short, addressing the urgent need for faster interventions in mental health care.
Ketamine infusion therapy involves the intravenous administration of low-dose ketamine, a medication originally developed as an anesthetic in the 1960s. Over time, research has revealed its potential to promote synaptogenesis and neural plasticity in the brain, leading to quick improvements in mood. Unlike standard antidepressants that may take weeks to work, studies from the PMC article on ketamine therapy show response rates within hours for many patients, with significant reductions in depressive symptoms. The FDA has approved ketamine derivatives for certain uses, while off-label applications target disorders like treatment-resistant depression and anxiety. Common misconceptions portray ketamine as merely a party drug, but in clinical settings, ketamine infusion is tightly controlled, safe, and supervised to harness its therapeutic benefits for ketamine for depression and ketamine for anxiety.
At Charleston Ketamine Center in Charleston, South Carolina, patients receive personalized IV ketamine treatment protocols in a supervised outpatient environment. Led by experienced clinicians, the center combines precision dosing with behavioral support, ensuring comprehensive care tailored to individual needs. They also integrate aesthetic services to support overall well-being.
This guide explores the fundamentals of ketamine's mechanisms, delves into practical considerations for therapy, and covers advanced applications, empowering you with knowledge for informed decisions about this transformative treatment.
Fundamentals of Ketamine Therapy
In the evolving landscape of mental health care, ketamine for depression has emerged as a promising option for those seeking rapid relief. Ketamine infusion therapy, originally developed as a dissociative anesthetic, is now repurposed in psychiatry to address severe mood disorders. At centers like the Charleston Ketamine Center in South Carolina, this approach offers hope for patients with treatment-resistant conditions, blending innovative science with supervised clinical care.
Ketamine serves as a foundational tool in ketamine-based mental health treatment, particularly for individuals who have not responded to conventional therapies. As a non-competitive antagonist of the NMDA receptor, it disrupts typical glutamate signaling in the brain. This leads to a compensatory surge in glutamate release, which activates AMPA receptors and promotes synaptogenesis, or the formation of new neural connections. In essence, ketamine helps rewire brain circuits disrupted by chronic depression or anxiety, fostering neural plasticity that can restore emotional balance. Studies, including those from the referenced PMC article, highlight how this mechanism provides antidepressant effects within hours, contrasting sharply with slower-acting options.
Understanding these mechanisms underscores the value of comparing ketamine to traditional antidepressants, as it reveals distinct pathways to relief that can guide patient choices. For those in Charleston exploring options, such insights clarify why ketamine might suit cases needing quick intervention.
| Aspect | Ketamine Infusion Therapy | Traditional Antidepressants (e.g., SSRIs) |
|---|---|---|
| Onset of Effects | Hours to days | Weeks to months |
| Mechanism | Synaptogenesis and neural plasticity | Serotonin reuptake inhibition |
| Common Side Effects | Dissociation, nausea (short-term) | Weight gain, sexual dysfunction (long-term) |
| Treatment Duration | Series of infusions over weeks | Daily pills ongoing |
This comparison illustrates ketamine's advantages in delivering fast-acting relief through unique neural pathways, making it ideal for urgent cases of treatment-resistant depression. Traditional options, while effective for many, often require prolonged commitment with gradual benefits. Data from the PMC article supports ketamine's rapid efficacy, showing response rates up to 70% in trials for mood disorders.
Building on these differences, standard infusion protocols for mood disorders at clinics like Charleston Ketamine Center involve precise dosing, typically 0.5 mg/kg administered intravenously over 40 minutes. Patients undergo 6-8 initial sessions spaced over several weeks, with ongoing maintenance as needed. During each infusion, vital signs such as blood pressure and heart rate are closely monitored to ensure safety. The PMC article reports low adverse event rates, with serious incidents under 5%, affirming the procedure's overall security when supervised.
Common side effects are generally mild and transient, resolving shortly after treatment:
- Dissociation or altered perception, likened to a brief dream-like state
- Temporary increases in blood pressure or nausea
- Mild sedation during the infusion
These effects highlight the importance of professional oversight. For ketamine for anxiety applications, similar protocols apply, targeting heightened neural overactivity to promote calm.
At the Charleston Ketamine Center in Mount Pleasant, South Carolina, therapy begins with thorough pre-screening to tailor plans for conditions like depression and anxiety. This local emphasis on personalized, supervised care ensures accessibility and efficacy for regional patients.
As these fundamentals reveal ketamine's potential, deeper exploration into clinical outcomes and patient experiences follows, providing a fuller picture of its role in modern psychiatry.
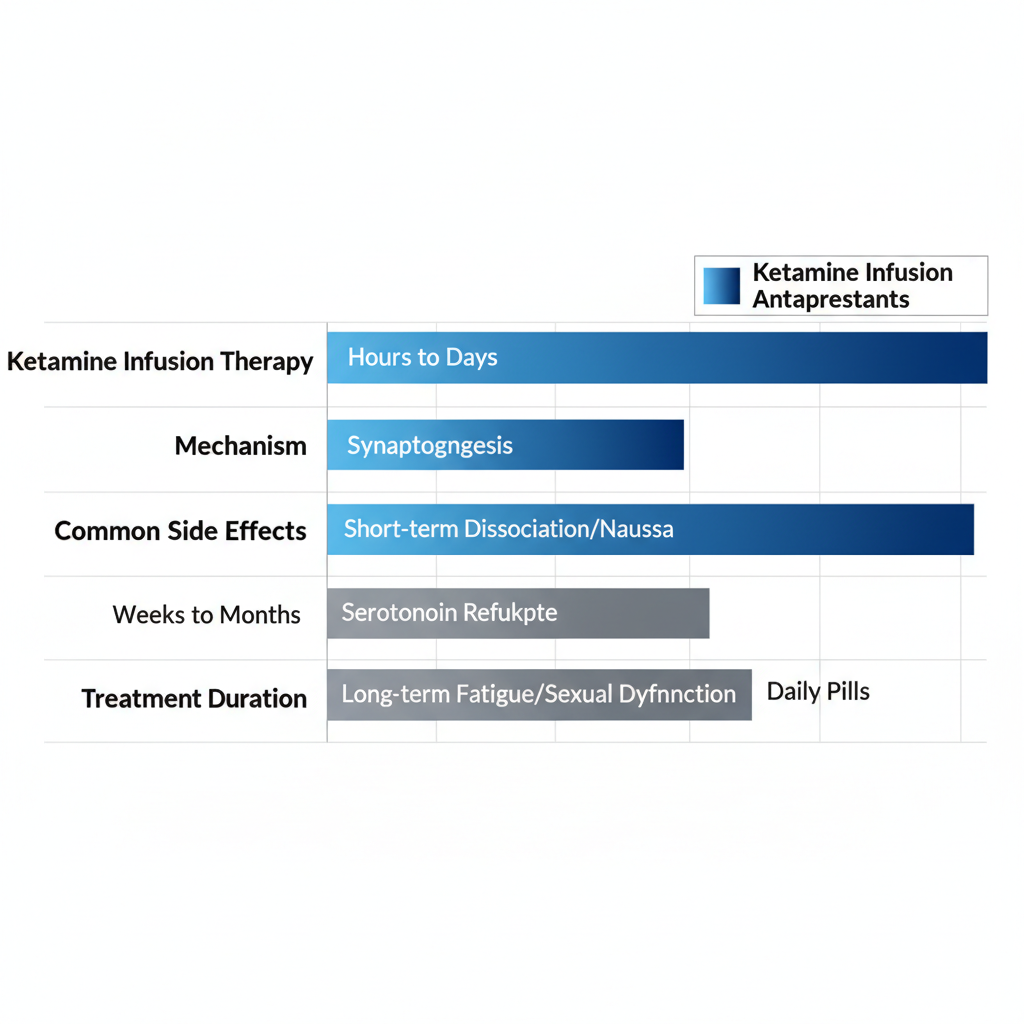
Bar chart: Ketamine vs. traditional antidepressants comparison
This visual reinforces how ketamine stands out for speed and innovation, aiding those in Charleston, South Carolina, in weighing therapeutic paths.
Mechanisms and Clinical Evidence of Ketamine
Ketamine infusion therapy stands out for its rapid effects on mental health conditions like depression and anxiety. At facilities such as the Charleston Ketamine Center in Mount Pleasant, South Carolina, this treatment leverages unique neurobiological pathways to foster brain changes that traditional antidepressants often cannot achieve. This section delves into how ketamine promotes neural plasticity and reviews key clinical evidence supporting its use.
How Ketamine Promotes Brain Plasticity
Ketamine works primarily by modulating the brain's glutamate system, a key neurotransmitter involved in learning and mood regulation. Unlike conventional antidepressants that target serotonin or norepinephrine, ketamine blocks NMDA receptors, leading to a surge in glutamate release. This cascade activates AMPA receptors, triggering downstream signaling that enhances synaptogenesis--the formation of new neural connections in areas like the prefrontal cortex, which is often impaired in depression and anxiety.
Central to this process is the upregulation of brain-derived neurotrophic factor (BDNF), a protein that supports neuron survival and growth. Studies indicate that ketamine rapidly increases BDNF levels, promoting neuroplasticity via ketamine mechanisms that restore synaptic density within hours. For patients with treatment-resistant depression, this means quicker mood stabilization as weakened neural circuits rebuild, alleviating persistent symptoms.
In anxiety disorders, similar plasticity effects quiet overactive fear circuits in the amygdala. At the Charleston Ketamine Center, protocols emphasize precision dosing to maximize these benefits while minimizing side effects. However, limitations exist, such as the need for repeated infusions due to ketamine's short half-life, and ongoing research explores long-term synaptic stability.
The following table compares key brain pathways activated by ketamine versus placebo, highlighting differences in neural response:
| Pathway | Ketamine Activation | Placebo Activation | Outcome |
|---|---|---|---|
| Glutamate Release | High | Low | Enhanced AMPA signaling |
| NMDA Blockade | Strong | None | Reduced excitotoxicity |
| BDNF Upregulation | Rapid (within hours) | Minimal | Synaptogenesis and plasticity |
This comparison underscores ketamine's unique ability to jumpstart neural repair, drawing from neurobiology insights in peer-reviewed sources. Such targeted activation explains why evidence-based infusion treatments yield faster results than placebo in preclinical models. Integrating these mechanisms with behavioral support amplifies outcomes, particularly when combined with ketamine assisted psychotherapy, which helps patients process newfound emotional flexibility.

Ketamine's brain plasticity mechanisms and clinical evidence
These visual representations of pre- and post-treatment neural changes illustrate how ketamine fosters resilience against stress-related disorders. For those seeking ketamine for depression or anxiety in the Charleston area, understanding this science informs expectations for therapy integration and sustained relief.
Evidence from Clinical Studies
Clinical trials have robustly demonstrated ketamine's efficacy, particularly for treatment-resistant conditions. Randomized controlled trials (RCTs) show that ketamine for depression achieves response rates of 70-80% in patients unresponsive to multiple antidepressants, with effects onset as early as 24 hours post-infusion. A meta-analysis from PMC sources reports remission rates around 50% in severe cases, far surpassing placebo outcomes and addressing the question of how effective ketamine is for treatment-resistant depression.
For anxiety, studies reveal 60-75% symptom reduction, with rapid relief in generalized anxiety and PTSD. Key findings include decreased Hamilton Anxiety Rating Scale scores within days, answering how ketamine helps with anxiety disorders through dampened hyperarousal. Small sample sizes remain a limitation, but larger trials confirm durability up to two weeks post-treatment.
- A 2018 RCT (n=73) on treatment-resistant depression found 71% response after six infusions, with BDNF elevations correlating to mood improvements (PMC-cited).
- Anxiety-focused trials, like a 2020 study on social anxiety, reported 65% reduction in symptoms via single-dose ketamine, emphasizing quick action for acute distress.
- Integration with psychotherapy enhances long-term gains, as seen in protocols at Charleston Ketamine Center, where follow-up sessions build on infusion-induced insights.
Biomarkers like elevated BDNF validate these results, linking biological changes to clinical relief. While promising, studies stress supervised administration to manage transient side effects like dissociation.
The table below summarizes ketamine efficacy across depression and anxiety, based on PMC meta-analyses:
| Condition | Response Rate | Study Duration | Key Findings |
|---|---|---|---|
| Depression | 70-80% | 1-2 weeks post-infusion | Rapid remission in 50% of resistant cases; BDNF-linked synaptogenesis |
| Anxiety | 60-75% | 1-2 weeks post-infusion | Quick symptom relief; reduced amygdala activity |
These outcomes highlight ketamine's versatility, with higher responses in depression due to stronger prefrontal impacts. For Charleston patients, this data supports personalized plans at the Ketamine Center, bridging scientific evidence to practical, outpatient care. Ongoing research refines dosing for optimal neural and behavioral synergy, promising broader applications in mood disorders.
Practical Guide to Ketamine Infusion Sessions
Embarking on iv infusion therapy at Charleston Ketamine Center in South Carolina offers a structured path to relief for treatment-resistant conditions. This guide demystifies the process, from initial steps to recovery, ensuring you feel prepared and supported throughout your journey.
Preparing for Your First Infusion
Starting ketamine infusion therapy requires thorough preparation to maximize safety and effectiveness. Begin with a comprehensive medical screening at Charleston Ketamine Center, where licensed professionals review your medical history, current medications, and mental health goals. This consultation, often free, helps tailor the treatment plan to your needs, addressing conditions like depression or anxiety.
Key Preparation Steps:
- Schedule a Consultation: Contact the center at (843) 324-6726 to book your initial assessment. Discuss symptoms and expectations openly.
- Fasting Guidelines: Avoid solid foods for at least six hours before the session, but stay hydrated with clear liquids to prevent nausea.
- Arrange Transportation: Plan for a ride home, as effects may linger, impairing your ability to drive.
- What to Bring: Pack comfortable clothing, a water bottle, and any preferred music playlist for relaxation. Items like a journal for post-session reflections can enhance integration.
These steps align with clinical guidelines from sources like PMC articles on ketamine protocols, emphasizing pre-treatment evaluation to minimize risks. Patients often report feeling more at ease after this phase, with one noting, "The screening made me confident in the center's expertise."
| Element | Standard Protocol | Personalized at Charleston Ketamine Center |
|---|---|---|
| Dosing | Fixed 0.5 mg/kg | Tailored 0.5-1 mg/kg based on individual response and weight |
| Monitoring | Basic vitals | Continuous vitals, psychological observation, and adjustments by licensed staff |
| Follow-Up | Standard check-ins | Customized integration sessions and maintenance scheduling |
During and After the Infusion
Once prepared, your session at Charleston Ketamine Center unfolds in a serene, outpatient environment designed for comfort. You'll settle into a recliner in a private room, with options for soothing music or dim lighting to foster relaxation. The infusion itself, a session-based ketamine treatment, typically lasts 40-60 minutes, administered intravenously under close supervision.
During the Infusion:
- Dosage Administration: For ketamine for anxiety, dosing ranges from 0.5-1 mg/kg, adjusted precisely to your profile. This promotes rapid neural effects without overwhelming intensity.
- Monitoring Process: Licensed staff track vital signs continuously, including heart rate, blood pressure, and oxygen levels, per PMC-recommended standards. This real-time oversight ensures a secure experience, addressing any mild dissociative sensations promptly.
- Patient Experience: Many describe a dream-like state with vivid insights, particularly helpful for those seeking ketamine for depression. The center's team provides gentle guidance if needed.
Immediately after, you'll rest in a recovery area for 30-60 minutes as effects subside. Common after-effects include mild dizziness or euphoria, which fade quickly. Hydration and light snacks help, and staff offer insights into what you experienced.
Post-Infusion Care:
- Immediate Follow-Up: Schedule integration sessions to process insights, boosting long-term benefits. Effects for anxiety relief often emerge within hours, lasting days to weeks.
- Maintenance Plan: Booster infusions every 1-4 weeks maintain progress, with the center tracking your response.
- Insurance and Accessibility: While coverage varies, self-pay options make ketamine therapy in Charleston, South Carolina accessible. Inquire during consultation for details.
| Effect Type | Immediate (0-24 Hours) | Long-Term (Weeks-Months) |
|---|---|---|
| Mood Lift | Rapid reduction in anxiety | Sustained elevation via neural plasticity |
| Side Effects | Mild dissociation | Minimal with proper spacing and integration |
| Duration | 1-7 days | Up to 3 months with maintenance |
Advanced Applications and Outcomes of Ketamine
Ketamine infusion therapy represents a transformative approach for patients seeking relief from persistent mental health challenges. At Charleston Ketamine Center in Charleston, South Carolina, advanced protocols extend beyond initial treatments to address complex conditions through precision dosing and holistic care. This section explores how these enhanced ketamine protocols yield lasting benefits and integrate with broader therapeutic strategies.
Specialized applications of ketamine target intricate disorders such as bipolar disorder and post-traumatic stress disorder. For instance, in cases of treatment-resistant bipolar depression, low-dose infusions promote mood stabilization without exacerbating manic episodes. Similarly, ketamine for anxiety offers rapid symptom reduction for those with generalized anxiety disorder, often within hours of administration. Ketamine for depression proves particularly effective in severe, refractory cases, where traditional antidepressants fall short. Hypothetical patient scenarios at the center illustrate this: a veteran with PTSD experiences diminished hypervigilance after a series of sessions, enabling engagement in daily activities. These integrated mental health infusions combine with cognitive behavioral techniques to amplify results, fostering resilience in complex presentations.
Outcomes from advanced ketamine therapy emphasize both immediate relief and enduring neural changes. Short-term effects include swift alleviation of depressive symptoms, with many patients reporting enhanced clarity and reduced suicidal ideation post-infusion. Long-term benefits stem from sustained synaptogenesis, promoting neural remodeling that supports ongoing emotional regulation. According to PMC studies, up to 70% of participants in follow-up trials achieve remission at the six-month mark, underscoring the therapy's potential for relapse prevention.
Ketamine Outcomes: Short-Term vs Long-Term
| Phase | Effects | Duration | Maintenance Needs |
|---|---|---|---|
| Short-Term | Rapid mood lift | Hours to days | Initial series of 6 infusions |
| Long-Term | Neural remodeling | Weeks to months | Booster every 4-6 weeks |
This comparison reveals how short-term gains provide quick momentum, while long-term neural adaptations require strategic maintenance to sustain benefits. For patients at local clinics like Charleston Ketamine Center, progress monitoring tools such as mood journals and follow-up assessments guide booster scheduling, ensuring optimal therapeutic trajectories. Relapse prevention strategies, including lifestyle integration, further enhance durability, with ethical oversight prioritizing informed consent and minimal side effects.
Integration with complementary therapies elevates ketamine's efficacy. Pairing infusions with psychotherapy allows patients to process insights gained during treatment, deepening emotional breakthroughs. At the center, this extends to medical aesthetics, where procedures like neurotoxins complement mental health gains by boosting self-esteem. For example, a client undergoing ketamine for depression might combine sessions with dermal fillers for a holistic rejuvenation, addressing both internal and external well-being. Such multimodal approaches, supported by PMC research on combined therapies, yield synergistic improvements in quality of life.
Looking ahead, future research at facilities like Charleston Ketamine Center promises refined protocols for diverse populations. Key directions include:
- Optimizing dosing for geriatric patients with anxiety.
- Exploring ketamine's role in addiction recovery alongside mood disorders.
- Advancing biomarkers for personalized treatment predictions.
Ethical considerations, such as equitable access and long-term safety monitoring, remain paramount. These innovations position ketamine as a cornerstone in evolving mental health care.
As these advanced applications demonstrate, ketamine therapy in Charleston, South Carolina, offers hope for sustained recovery, paving the way for informed discussions on personalized care plans.
Common Questions About Ketamine Therapy
Considering ketamine infusion therapy for mental health support? Charleston Ketamine Center addresses frequent patient inquiries below, focusing on practical aspects for those seeking relief from treatment-resistant conditions.
Is ketamine infusion therapy covered by insurance?
Most insurance plans do not cover it, making it primarily out-of-pocket, though financial assistance programs may help. Our team can guide you on options during a free consultation.
How long do the effects of ketamine for depression last?
Benefits often persist 1-2 weeks, with booster sessions recommended for sustained relief. This rapid action helps bridge gaps in traditional treatments.
Are there clinical studies on ketamine for anxiety?
Yes, studies like those in PMC show ketamine's efficacy in reducing anxiety symptoms quickly, with strong safety profiles under medical supervision.
Where can I access ketamine therapy in Charleston, South Carolina?
At Charleston Ketamine Center, 1948 Long Grove Drive #2, Mount Pleasant. Call (843) 324-6726 or email coastalketaminechs@gmail.com to schedule.
Does ketamine treatment help with both anxiety and depression?
Absolutely, it targets mood disorders by promoting neural plasticity, offering fast symptom relief for many patients.
Embracing Ketamine Therapy for Mental Wellness
Ketamine infusion therapy offers transformative relief for those battling treatment-resistant conditions, with rapid effects on mood stabilization and synaptogenesis promoting neural growth. Backed by clinical evidence from PMC studies, its safety profile shines in supervised settings for ketamine for depression and ketamine for anxiety. Innovative infusion treatments at Charleston Ketamine Center integrate holistic support, making Charleston mental health solutions accessible and effective.
Ready to embrace change? Schedule your free consultation today at our Mount Pleasant clinic, located at 1948 Long Grove Drive #2, South Carolina. Call (843) 324-6726 or email coastalketaminechs@gmail.com to start your personalized journey toward wellness.
As psychiatric advancements evolve, ketamine therapy in Charleston, South Carolina, heralds a brighter, more resilient future for mental health.