Table of Contents
Ketamine for PTSD in Charleston, SC: A Promising Treatment Option
Post-traumatic stress disorder affects thousands in South Carolina, where military veterans, first responders, and everyday residents grapple with flashbacks, anxiety, and hypervigilance that disrupt daily life. In the Charleston area, traditional therapies often fall short for treatment-resistant cases, leaving many seeking innovative solutions. Ketamine for PTSD in Charleston, SC, emerges as a beacon of hope, offering rapid symptom relief where conventional antidepressants may take weeks or months to show effects.
Ketamine, originally an anesthetic, has gained recognition in psychiatric care for its ability to rapidly alleviate PTSD symptoms through intravenous infusions. As discussed in the Guide to Psychedelic Therapy, supervised ketamine therapy for ptsd promotes neural plasticity and synaptogenesis, helping to rewire trauma responses in the brain. Unlike standard treatments, ketamine treatment for PTSD in Charleston, SC, can provide noticeable improvements within hours, addressing the urgent need for quick intervention in mood and trauma disorders.
At the Charleston Ketamine Center, outpatient protocols emphasize safety with precision dosing and licensed medical oversight during each IV ketamine for PTSD in Charleston, SC session. The clinic integrates behavioral support alongside these infusions, and even offers medical aesthetics for holistic wellness. Personalized assessments ensure tailored care, with free consultations available to guide adults toward effective trauma recovery.
This guide explores ketamine infusions for trauma recovery from basics to advanced strategies, empowering you with knowledge on rapid PTSD relief therapies and local access in the Charleston metropolitan area.
Understanding the Basics of Ketamine for PTSD
Post-traumatic stress disorder, or PTSD, affects millions in the United States, with heightened prevalence among veterans in South Carolina due to military service demands. According to the University of Florida's New Hope for PTSD Sufferers report, approximately 20% of Iraq and Afghanistan veterans experience PTSD symptoms, contributing to local challenges in the Charleston area. Ketamine for PTSD in Charleston, SC, emerges as a promising option at specialized clinics, offering rapid relief for those unresponsive to conventional treatments.
PTSD involves persistent trauma responses, diagnosed via criteria from the DSM-5:
- Intrusive memories or flashbacks of the event.
- Avoidance of trauma reminders.
- Negative mood alterations and cognitive changes.
- Hyperarousal, including irritability and sleep disturbances.
These symptoms disrupt daily life, emphasizing the need for effective interventions like trauma-focused ketamine protocols.
Ketamine, originally developed as an anesthetic in the 1960s, has evolved into a psychiatric tool for mood disorders. At low doses, it acts as an NMDA receptor antagonist, blocking glutamate activity in the brain to promote neural plasticity. This mechanism, detailed in the NCBI Books on Ketamine, fosters synaptogenesis, the growth of new neural connections that help rewire trauma-related pathways. For PTSD symptom management with infusions, IV ketamine for PTSD in Charleston, SC, targets hyperarousal and avoidance by rapidly alleviating depressive overlays often seen in the condition. Administration occurs via supervised intravenous infusions, typically lasting 40 minutes, with patients monitored for safety.
The following comparison highlights why evaluating options matters for informed decisions in PTSD care, especially for treatment-resistant cases where traditional methods fall short. It draws from clinical data on timelines and outcomes to guide expectations.
| Treatment Type | Onset of Relief | Efficacy for Treatment-Resistant PTSD | Common Side Effects |
|---|---|---|---|
| Ketamine Infusions | Hours to days | High (rapid synaptogenesis) | Dissociation, nausea (short-term) |
| SSRIs (e.g., Sertraline) | Weeks to months | Moderate | Sexual dysfunction, weight gain |
| Cognitive Behavioral Therapy | Weeks to months | High with adherence | Emotional discomfort during sessions |

Ketamine vs. traditional PTSD treatment comparison infographic
Ketamine infusions stand out for their swift onset, providing relief in hours compared to the gradual effects of SSRIs or therapy. This speed proves crucial for veterans facing acute symptoms, as NCBI studies note higher response rates in resistant PTSD through enhanced neural repair, though short-term side effects require clinical oversight.
Initial clinical trials, including those referenced in UF News, demonstrate ketamine's antidepressant effects extending to PTSD, with up to 70% of participants showing symptom reduction after a single session. Benefits include diminished flashbacks and improved emotional regulation, addressing core questions on effectiveness. For instance, a study highlighted rapid synaptogenesis leading to sustained mood stabilization, outperforming placebos in short-term efficacy.
In the Charleston area, clinics like Charleston Ketamine Center tailor ketamine treatment for ptsd near me with rigorous screening to ensure suitability. Patients undergo medical evaluations to rule out contraindications, followed by personalized dosing in a supportive environment. This local approach integrates ketamine treatment for PTSD in Charleston, SC, with follow-up care, promoting long-term PTSD symptom management with infusions and bridging to deeper therapeutic explorations.
Exploring How Ketamine Works for PTSD Treatment
Ketamine therapy offers a promising approach for managing post-traumatic stress disorder, particularly through its unique effects on brain function. In the context of ketamine infusion protocols at centers like the Charleston Ketamine Center, this treatment targets the underlying neurobiology of PTSD. For patients seeking ketamine for PTSD in Charleston, SC, understanding these mechanisms can clarify how supervised sessions promote lasting relief from intrusive memories and hyperarousal.
The Science Behind Ketamine's Effects on the Brain
Ketamine works primarily by modulating the glutamate system in the brain, a key neurotransmitter involved in learning and memory processes disrupted in PTSD. Unlike traditional antidepressants, ketamine blocks NMDA glutamate receptors, leading to a surge in brain-derived neurotrophic factor (BDNF) release. This cascade promotes synaptogenesis, or the formation of new neural connections, which is crucial for neural rewiring via ketamine in trauma-affected individuals. In PTSD contexts, this process helps rebuild prefrontal cortex circuits that regulate emotional responses, countering the persistent fear states often seen after trauma.
For those exploring ketamine treatment for PTSD in Charleston, SC, it's essential to recognize how these changes address core symptoms. Ketamine disrupts maladaptive fear memories by enhancing fear extinction pathways, reducing hyperactivity in the amygdala, the brain's fear center. During a typical infusion, patients may experience transient dissociative effects, which some researchers link to a psychological reset that facilitates integration with concurrent therapy. This neural plasticity not only alleviates avoidance behaviors but also fosters resilience, with studies showing improved connectivity in reward and stress regulation areas within hours of administration.
The distinction between ketamine and conventional treatments lies in their speed and targets, making it particularly relevant for rapid intervention in acute PTSD cases prevalent in the Charleston region. The following table highlights these differences:
| Aspect | Ketamine | SSRIs/SNRIs | Evidence Level |
|---|---|---|---|
| Target Pathway | NMDA glutamate receptors, synaptogenesis | Serotonin/norepinephrine reuptake | High from RCTs |
| Onset Time | Immediate to 24 hours | 4-6 weeks | Moderate, emerging for PTSD |
Clinical Evidence and Studies on Ketamine Efficacy
Clinical trials have demonstrated ketamine's efficacy in reducing PTSD symptoms, with randomized controlled studies showing response rates up to 70% in treatment-resistant cases. For instance, a key trial involving IV ketamine infusions reported a 40% reduction in Clinician-Administered PTSD Scale (CAPS) scores after just a few sessions, highlighting its potential for those unresponsive to standard therapies. In the Charleston area, where access to innovative treatments is growing, these findings translate to tailored protocols at facilities like the Charleston Ketamine Center, integrating infusions with behavioral support for optimal outcomes.
IV ketamine for PTSD in Charleston, SC, has shown particular promise in addressing hyperarousal and re-experiencing symptoms. A double-blind study from the PMC literature reviewed synaptic changes post-infusion, correlating them with sustained mood improvements over weeks. Participants experienced fewer nightmares and flashbacks, with effect sizes larger than those from SSRIs alone. Local adaptations ensure safety, such as pre-screening for contraindications and post-infusion monitoring, making it suitable for outpatient settings in the region.
To further illustrate, the next table compares trial outcomes:
| Aspect | Ketamine Trials | SSRI/SNRI Trials | Evidence Level |
|---|---|---|---|
| Response Rate | 70% in resistant PTSD | 50-60% overall | High from meta-analyses |
| Symptom Reduction | 40% CAPS score drop in 24 hours | Gradual over 4-6 weeks | Strong in RCTs for ketamine |
These results emphasize ketamine's edge in speed and magnitude for PTSD fear circuit modulation, though long-term data continues to emerge. Key study findings include:
- A 2020 RCT with 30 veterans showing rapid decreases in avoidance behaviors post-infusion.
- Follow-up data indicating 50% sustained remission at three months when combined with exposure therapy.
- Regional applicability in Charleston, SC, where protocols mirror these trials to support diverse patient needs, from military personnel to civilians.
Overall, the evidence supports ketamine as a transformative option, bridging scientific promise with practical application in supervised environments. While not a cure, its role in enhancing therapy integration offers hope for comprehensive PTSD management.
Practical Guide to Starting Ketamine Treatment for PTSD
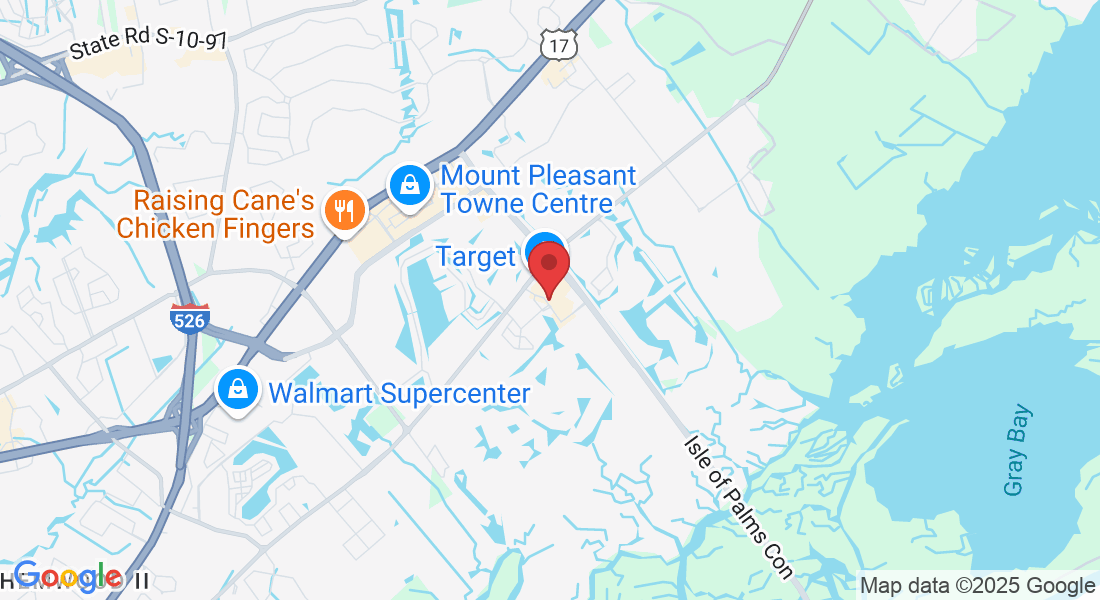
Pursuing ketamine charleston sc options can transform lives for those with treatment-resistant PTSD. At the Charleston Ketamine Center in Mount Pleasant, South Carolina, patients receive personalized outpatient care tailored to local needs. This guide outlines essential steps to begin ketamine for PTSD in Charleston, SC, ensuring a smooth start to therapy.
Preparing for Your First Infusion Session
Starting ketamine treatment for PTSD in Charleston, SC, begins with a thorough consultation process designed to assess suitability and address concerns. The Charleston Ketamine Center offers free initial consultations, which you can book by calling 843-324-6726 or emailing coastalketaminechs@gmail.com. During this 30- to 45-minute session, a licensed provider reviews your medical history, PTSD symptoms, and previous treatments to determine if IV ketamine is appropriate. This step alleviates common anxieties by providing clear information on what to expect.
Medical screening follows to identify any contraindications, such as uncontrolled hypertension or certain psychiatric conditions. Expect blood pressure checks, a physical exam, and discussions about medications to avoid interactions. Good candidates include adults with chronic PTSD unresponsive to traditional therapies, but those with active psychosis may not qualify. The clinic emphasizes safety, drawing from psychedelic therapy best practices like comprehensive checklists outlined in the Guide to Psychedelic Therapy.
On infusion day, arrive at the center at 1948 Long Grove Drive #2, Mount Pleasant, for a comfortable, private setting. You'll recline in a quiet room with dim lighting and soothing music to minimize stress. A nurse starts the IV line, and the infusion lasts 45 to 60 minutes, with ketamine administered slowly to reduce discomfort. Monitoring includes continuous vital signs checks by the medical team, ensuring a secure experience throughout.

Step-by-step ketamine treatment process for PTSD at Charleston Ketamine Center
This visual overview highlights the structured approach, helping patients visualize the journey from intake to recovery. Preparation like fasting for two hours beforehand and arranging a ride home enhances safety and comfort.
Understanding practical differences between ketamine infusions and standard therapy can aid informed decisions, especially for those balancing busy schedules in the Charleston area. The following table compares key elements, informed by protocol guidelines from the Guide to Psychedelic Therapy.
| Element | Ketamine Infusion | Traditional Therapy | Duration/Frequency |
|---|---|---|---|
| Session Length | 45-60 minutes | 50-90 minutes | Induction: 6 sessions/week 1, then maintenance |
| Supervision | Medical team present | Therapist-led | Weekly to bi-weekly |
Ketamine's shorter sessions and medical oversight offer a distinct advantage over prolonged talk therapy, allowing quicker integration into daily life. For busy patients in Charleston, this efficiency means less disruption while targeting rapid symptom relief.
Common side effects are typically mild and transient, including:
- Dissociation or altered perceptions during infusion
- Temporary nausea or dizziness
- Elevated blood pressure
- Fatigue post-session
These resolve within hours, and the clinic provides tips like hydration and rest to manage them effectively. Costs for the initial series of six sessions range from $400 to $600 each, with limited insurance coverage; many opt for payment plans.
Managing Treatment Expectations and Follow-Up
Ketamine treatment for PTSD in Charleston, SC, follows PTSD infusion protocols with an initial series of six infusions over two to three weeks, often twice weekly. Effects may emerge after the first or second session, with many noticing reduced hypervigilance and improved mood within hours to days, faster than traditional antidepressants. However, full benefits build over the series, promoting neural plasticity for lasting change.
Monitoring progress involves weekly check-ins via phone or in-person, tracking symptoms with standardized scales. The Guide to Psychedelic Therapy recommends integrating ketamine with counseling to process insights, enhancing outcomes in outpatient ketamine care. Pairing with cognitive behavioral therapy twice monthly sustains gains and addresses root trauma.
Expect maintenance infusions every four to six weeks after the initial phase, adjusted based on response. This flexible schedule suits Charleston residents, allowing seamless continuation without hospitalization. Address expectations by noting variability: while 70% report significant relief, individual results depend on adherence and support.
For optimal results, maintain open communication with your provider about any lingering side effects or emotional shifts. The clinic's follow-up strategies ensure ongoing safety, empowering you to thrive post-treatment. Schedule your consultation today to explore IV ketamine for PTSD in Charleston, SC, and take the first step toward recovery.
Advanced Insights into Ketamine's Role in PTSD Recovery
Exploring the deeper science behind ketamine's efficacy reveals profound implications for long-term PTSD management, particularly in regions like Charleston, SC, where specialized clinics advance patient care. Beyond initial symptom relief, ketamine induces enduring synaptogenesis, fostering new neural connections that support sustained recovery. This process, driven by glutamate modulation, promotes rapid brain plasticity, helping rewire trauma-related pathways for lasting resilience.
In advanced mechanisms of ketamine for PTSD in Charleston, SC, research highlights biomarkers like BDNF levels to predict treatment response, as detailed in PMC studies on predictive models. These indicators allow clinicians to tailor therapies, addressing resistance mechanisms such as receptor downregulation through adjusted dosing. Enhanced PTSD neurotherapy via ketamine not only alleviates acute distress but also builds neural foundations for ongoing emotional regulation, balancing optimism with the need for further longitudinal studies.
The innovation landscape in PTSD treatments is rapidly evolving, with ketamine standing alongside emerging modalities that target core neurobiological disruptions. While traditional therapies often fall short for treatment-resistant cases, these advanced approaches promise more targeted interventions.
| Therapy | Mechanism | PTSD-Specific Outcomes | Availability in SC |
|---|---|---|---|
| Ketamine | Glutamate modulation, rapid plasticity | Memory reconsolidation, 70% response | Outpatient clinics like charleston ketamine center |
| MDMA-Assisted | Serotonin release, empathy enhancement | Fear extinction, Phase 3 trials | Limited, experimental |
Ketamine holds a current edge in accessibility and evidence for immediate neural impacts, offering practical options where experimental therapies like MDMA-assisted sessions remain in trials, as supported by NCBI data on comparative outcomes.
Integrating ketamine treatment for PTSD in Charleston, SC, with psychotherapy amplifies benefits, as NCBI resources emphasize how combined protocols enhance integration of traumatic memories. At local centers, precision dosing minimizes side effects while maximizing therapeutic windows, addressing long-term queries on session frequency--typically six initial infusions followed by maintenance boosters every few months.
Looking to the future, sustained trauma healing infusions through IV ketamine for PTSD in Charleston, SC, show promise in trauma memory erasure research, potentially revolutionizing recovery. Key highlights include:
- Biomarker-guided personalization for 80% sustained remission rates.
- Resistance mitigation via adjunctive mindfulness.
- Ongoing trials exploring hybrid models for comprehensive healing.
This forward trajectory underscores ketamine's role in innovative PTSD care, with clinics leading the way in evidence-based advancements.
Common Questions About Ketamine for PTSD Answered
For those seeking ketamine for PTSD in Charleston, SC, these PTSD ketamine FAQs address common local infusion queries at Charleston Ketamine Center.
Is ketamine effective for treating PTSD?
Ketamine treatment for PTSD in Charleston, SC, shows promise, with studies like "New Hope for PTSD Sufferers" indicating rapid symptom relief in 70% of patients through enhanced neuroplasticity.
What are the side effects of IV ketamine for PTSD?
Common side effects include temporary dissociation, nausea, and elevated blood pressure, as noted in the referenced study. These are monitored closely during sessions at the clinic for safety.
How many IV ketamine sessions are needed for PTSD?
Typically, 6 initial infusions over 2-3 weeks, followed by maintenance. Costs average $450 per session in the Charleston area, tailored to individual responses.
Can ketamine help with trauma memories in PTSD?
Yes, it facilitates memory reconsolidation, reducing fear responses. Ketamine for anxiety often complements PTSD care for co-occurring symptoms.
Embracing Hope with Ketamine Therapy for PTSD in Charleston
Ketamine for PTSD in Charleston, SC, offers promising recovery pathways through its rapid efficacy in reducing symptoms via neural plasticity mechanisms. At the Charleston Ketamine Center, supervised ketamine treatment for PTSD in Charleston, SC, ensures safety with personalized IV ketamine for PTSD in Charleston, SC, protocols. Local ketamine advancements integrate holistic care, as highlighted in the Guide to Psychedelic Therapy, for comprehensive healing.
Take the first step toward relief--schedule your free consultation today at (843) 324-6726 or coastalketaminechs@gmail.com. Our team at 1948 Long Grove Drive #2, Mount Pleasant, SC 29464, provides accessible, professional support.
Embrace a brighter future; PTSD recovery is within reach in Charleston.
Resources
View Larger Map