Table of Contents
Understanding Stem Cell Therapy for Back Pain
Chronic back pain affects millions, turning daily activities into daunting challenges. Stem cell therapy for back pain emerges as a promising regenerative approach, using the body's own undifferentiated cells to repair damaged spinal tissues. At centers like Charleston Ketamine Center, which primarily offers ketamine infusions for mental health and aesthetic services, educational resources highlight complementary strategies like this for holistic pain management.
Back pain often stems from conditions such as degenerative disc disease, herniated discs, and osteoarthritis, impacting the spine's structure and function. These issues lead to inflammation and tissue breakdown, causing persistent discomfort in the lower back. According to foundational studies, up to 80% of adults experience back pain at some point, with traditional treatments like surgery or medications providing only temporary relief. Stem cell treatment lower back pain offers a non-invasive alternative, targeting root causes rather than symptoms.
Regenerative stem cell therapy back pain works by injecting stem cells into affected areas, where they act as repair crews for the spine. These cells reduce inflammation and promote tissue regeneration, potentially restoring disc height and alleviating nerve pressure. Early clinical trials report success rates of 60-70% in improving mobility and reducing pain, as they differentiate into needed cell types to heal chronic damage. This cellular therapy for chronic back issues appeals to those seeking safer options over invasive procedures.
While not a core service at facilities focused on mental wellness, regenerative medicine for spinal pain integrates well with broader care plans. Upcoming sections explore safety, effectiveness, and options in the Southeast US, helping you decide if this could fit your journey to relief.
Basics of Stem Cell Therapy for Back Pain
Chronic back pain affects millions, limiting daily activities and quality of life. Stem cell therapy for back pain emerges as a promising biological back pain management option, harnessing the body's natural healing abilities. This regenerative approach targets underlying issues like degeneration and inflammation, offering hope to those seeking alternatives to surgery or long-term medications. At centers providing comprehensive care, such as Charleston Ketamine Center in the US, patients can explore integrated wellness options distinct from traditional ketamine or aesthetic treatments.
Mesenchymal stem cells play a pivotal role in this therapy, acting like seed planters for tissue growth by modulating inflammation and promoting cartilage regeneration in the spine. These cells release growth factors that stimulate repair in damaged discs and joints, reducing pain and improving mobility. For back pain, they target areas like facet joints in the lower back, fostering long-term healing rather than temporary relief.
Common sources for mesenchymal stem cells include the patient's own body or donor materials, each with unique harvesting methods. Bone marrow aspirate involves drawing from the hip, while adipose tissue comes from fat via a quick procedure. Umbilical cord sources provide ready-to-use cells from donations. The following table compares these stem cell sources for back pain treatment, highlighting their pros, cons, and ideal applications.
| Stem Cell Source | Description | Pros | Cons | Best For Back Pain Type |
|---|---|---|---|---|
| Bone Marrow Aspirate | Harvested from patient's hip bone. | Autologous and rich in mesenchymal cells. Minimally invasive harvest; high regenerative potential. | Donor variability; procedure discomfort. | Chronic lower back degeneration. |
| Adipose Tissue | Extracted from abdominal fat via liposuction. | Abundant cells; easy access. Less painful harvest; good for inflammation. | Lower potency than bone marrow. | Soft tissue back injuries. |
| Umbilical Cord | Allogeneic from donor cords. | Immunoprivileged; off-the-shelf availability. High anti-inflammatory effects. | Regulatory concerns; potential rejection. | Disc-related back pain. |
Selecting the right source depends on the pain type and patient needs; for instance, bone marrow suits chronic degeneration due to its potency, while adipose works well for inflammatory soft tissue issues. Umbilical cord options excel in disc problems with their anti-inflammatory benefits, though regulatory aspects require careful consideration. This comparison helps tailor regenerative stem cell therapy back pain to individual cases, enhancing outcomes.
Discussions around these sources underscore their versatility in addressing various back conditions. Visual aids can further clarify choices, making complex options more accessible for patients evaluating treatments.

Comparison of stem cell sources for effective back pain treatment options
Protocols typically involve percutaneous delivery, where mesenchymal cell injections for spinal relief are guided by imaging into affected areas. Eligibility starts with MRI-confirmed degeneration, ensuring candidates have moderate to severe lower back issues without contraindications like active infections. Procedures occur outpatient, with minimal downtime, emphasizing safety through sterile techniques and follow-up monitoring to track progress and side effects.
Preliminary evidence from trials, as noted in stem cell therapy overviews, shows 60-70% pain improvement in participants with degenerative back pain. These studies highlight reduced inflammation and restored function, supporting stem cell treatment lower back pain as a viable option. Sessions cost $5,000 to $10,000, varying by source and clinic, with many reporting benefits lasting months to years. Safety profiles remain strong, with low complication rates, offering empathetic relief for enduring sufferers while similar applications, like stem cell therapy for knees, expand regenerative possibilities.
In-Depth Exploration of Stem Cell Treatments
Stem cell therapy represents a promising frontier in treating back pain, particularly for degenerative spinal conditions. By harnessing the body's regenerative potential, this approach addresses root causes rather than just symptoms. Integrative centers like the Charleston Ketamine Center in South Carolina complement these treatments with holistic wellness options, including botox for migraines for associated pain management, enhancing overall patient outcomes.
Mechanisms of Action in Spinal Repair
Stem cells exert their therapeutic effects through multiple pathways, primarily paracrine signaling and direct differentiation, which are crucial in repairing damaged spinal tissues. In stem cell therapy for back pain, mesenchymal stem cells derived from bone marrow or adipose tissue migrate to injury sites, secreting bioactive molecules like cytokines and growth factors. These paracrine effects reduce inflammation by modulating immune responses and promoting tissue homeostasis. Furthermore, stem cells can differentiate into chondrocytes or nucleus pulposus cells, aiding disc regeneration and restoring structural integrity.
Histological findings from studies, such as those in the Stem Cell Therapy Overview reference, demonstrate how these cells integrate into degenerative discs, fostering extracellular matrix production. This process also enhances neural plasticity, potentially alleviating neuropathic components of back pain. Compared to platelet-rich plasma (PRP) therapy, stem cells offer broader regenerative capacity due to their multipotency.
The following table outlines key mechanisms and their spinal applications:
| Effect | Description | Back Application |
|---|---|---|
| Anti-inflammatory | Stem cells release cytokines and exosomes to suppress pro-inflammatory mediators. | Reduces swelling in herniated discs, easing acute pain. |
| Regenerative | Differentiate into specialized cells and stimulate endogenous repair. | Repairs degenerated intervertebral discs in chronic cases. |
| Analgesic | Modulate pain signaling via neurotrophic factors. | Alleviates chronic lower back discomfort through neural modulation. |
These mechanisms highlight the multifaceted role of stem cells in spinal repair, supported by preclinical evidence showing improved disc hydration and reduced fibrosis. For patients under 65 without active cancer, this therapy typically requires 1-3 sessions, with risks like infection at 1-2% managed through sterile protocols.
Clinical Evidence and Outcomes
Clinical trials provide robust evidence for the efficacy of stem cell treatment lower back pain, particularly in degenerative disc disease and facet joint arthropathy. Randomized controlled trials (RCTs) reviewed in the Clinical Trials on Regenerative Therapy reference report responder rates of 65%, with 50-80% improvements in Visual Analog Scale (VAS) scores for pain and function. Patients often experience initial relief within 2-6 weeks, as stem cells integrate and exert anti-inflammatory effects, leading to sustained benefits over 12-24 months.
Long-term outcomes show reduced need for opioids and improved quality of life, with MRI evidence of disc rehydration in 70% of cases. For chronic back conditions, efficacy persists in 60% of participants at two years, outperforming conservative treatments like physical therapy alone. However, inefficacy occurs in about 20% due to advanced degeneration or poor candidacy, emphasizing the need for thorough screening.
This data addresses common concerns about timelines and durability, confirming stem cell interventions as viable for non-surgical candidates. Synergies with centers like Charleston Ketamine Center allow for combined protocols, integrating regenerative therapies with neuromodulation for comprehensive pain relief. Risks remain low, with no increased malignancy reported in trials, though monitoring is essential.
Variations in Regenerative Approaches
Regenerative stem cell therapy back pain varies by sourcing method, with autologous and allogeneic approaches offering distinct advantages for spinal applications. Autologous therapy uses the patient's own cells, harvested from bone marrow or fat, ensuring compatibility and minimizing immune reactions. Allogeneic options employ donor-derived cells, often from umbilical cord or placenta, providing off-the-shelf availability and potentially higher potency for certain conditions.
Bioactive cellular interventions for spine, such as these, target tissue engineering for pain relief by adapting to individual needs. Autologous methods suit personalized treatment for degenerative discs, while allogeneic excels in rapid deployment for acute inflammation. Compared to PRP, both provide superior cellular diversity, though session numbers remain 1-3.
The table below compares these approaches, drawing from clinical insights on efficacy and risks:
| Aspect | Autologous | Allogeneic | Back Pain Suitability |
|---|---|---|---|
| Source | Patient's own body | Donor tissue | Degenerative discs; personalized with low rejection |
| Efficacy | 70% pain reduction in trials | Similar outcomes; faster prep | Chronic inflammation cases; variable potency for facet joint issues |
| Risks | Harvest pain; infection low | Immune response; regulatory hurdles | Both suitable with monitoring |
Applying Stem Cell Therapy in Practice
Stem cell therapy offers a promising option for those suffering from chronic back pain, focusing on regeneration rather than just symptom management. This approach targets the root causes of discomfort, providing a practical path forward for patients who have not found relief through conventional methods. By understanding the process, individuals can make informed decisions about incorporating this treatment into their care plan.
Preparing for Treatment
Preparing for stem cell therapy for back pain begins with a thorough consultation at an orthopedic clinic specializing in regenerative medicine. Patients typically start by discussing their medical history, including the duration and intensity of lower back pain, with a qualified physician. This initial meeting often involves reviewing recent imaging like MRIs or X-rays to assess the extent of degenerative disc disease or other spinal issues. Screenings may include blood tests to ensure overall health and rule out contraindications such as active infections or certain autoimmune conditions.
Once eligibility is confirmed, pre-procedure steps focus on optimizing the body for treatment. Doctors recommend avoiding anti-inflammatory medications for a week prior, as these can interfere with the regenerative process. Hydration and a nutrient-rich diet support cellular health, while light activities like walking maintain mobility without strain. For someone like Sarah, a 45-year-old office worker with persistent lumbar pain from herniated discs, this preparation phase builds confidence and sets expectations for practical cellular regeneration for lumbar issues. Clinics across the US, particularly in orthopedic centers, guide candidates through these steps to ensure safety and efficacy. This structured approach answers key concerns about who qualifies, typically those with moderate pain unresponsive to conservative therapies.
Procedure Details and Recovery
The procedure for stem cell treatment lower back pain is outpatient and minimally invasive, usually lasting 30 to 60 minutes. Under local anesthesia and fluoroscopic guidance, physicians harvest stem cells from the patient's bone marrow or adipose tissue, process them in a lab to concentrate the viable cells, and then inject them directly into the affected spinal area. This targeted delivery promotes tissue repair and reduces inflammation at the source of pain.
Here are the key steps in the process:
- Harvesting: A small sample is taken from the iliac crest or abdomen using a needle aspiration technique.
- Processing: Cells are isolated and prepared in a sterile environment to maximize potency.
- Injection: Using real-time imaging, the solution is precisely placed into the spine or surrounding tissues.
- Monitoring: Vital signs are observed briefly post-injection before discharge.
Patients like Mark, who struggled with chronic sciatica, often report initial mild soreness similar to a deep tissue massage. Recovery emphasizes rest for the first 1-3 days, avoiding heavy lifting or strenuous activity. Full benefits emerge over 1-3 months as cells integrate and regenerate tissues. According to clinical trials, about 90% of patients return to normal activities within one week.
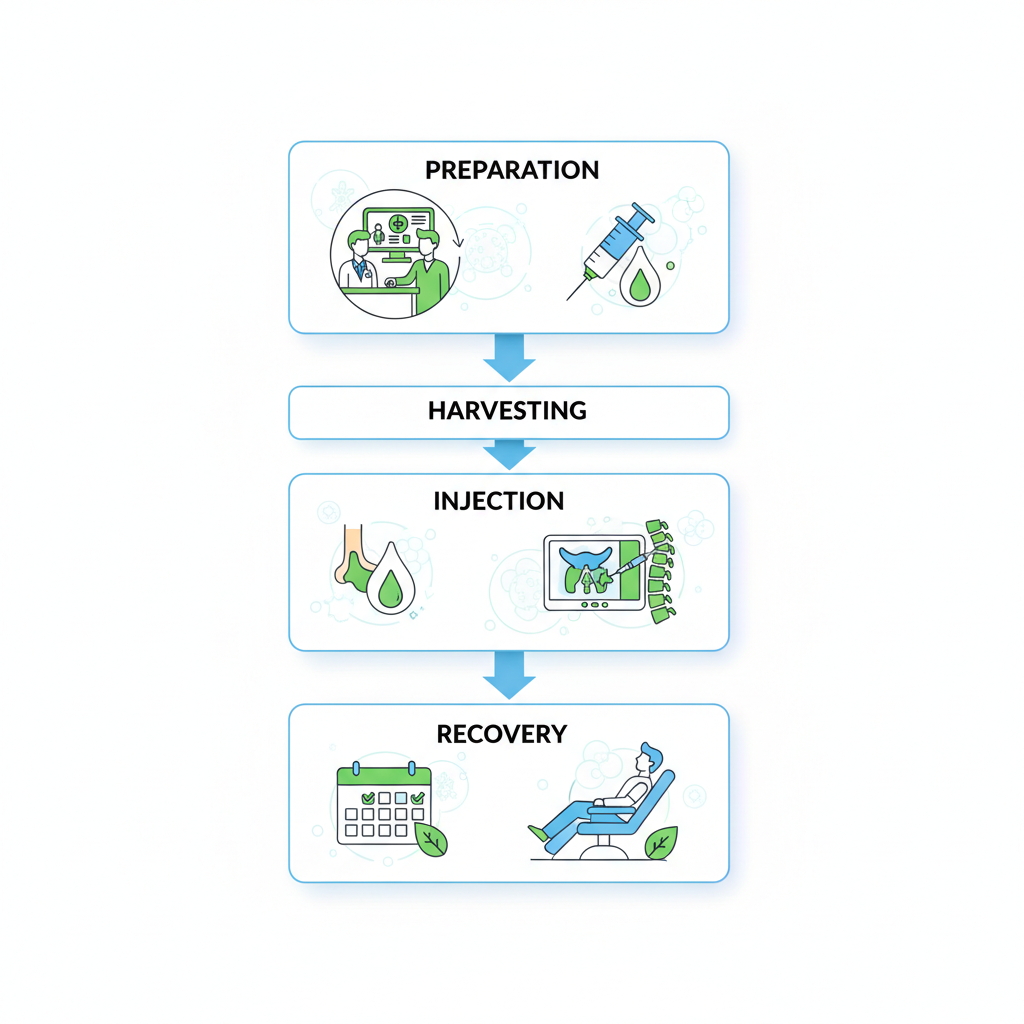
Step-by-step process of stem cell therapy for relieving back pain.
Post-treatment care includes gentle physical therapy to support healing. Bullet tips for optimal recovery:
- Stay hydrated and follow a anti-inflammatory diet rich in omega-3s.
- Attend follow-up appointments to monitor progress, typically 1-3 treatments spaced 4-6 weeks apart.
- Incorporate low-impact exercises like swimming after the initial downtime.
This phase addresses recovery time questions, with most experiencing significant relief without the long interruptions of more invasive options.
Comparing stem cell therapy to traditional back pain treatments highlights its unique benefits for chronic conditions. This evaluation helps patients weigh options based on their lifestyle and pain severity, drawing from established trial protocols that emphasize regenerative potential over symptomatic relief.
| Treatment | Invasiveness | Recovery Time | Efficacy for Chronic Pain | Cost Range |
|---|---|---|---|---|
| Stem Cell Injection | Minimally invasive | 1-2 days | 60-80% improvement | $5k-$10k |
| Spinal Surgery | Highly invasive | Weeks to months | 70% success but risks | $20k+ |
| Medications/PT | Non-invasive | Ongoing | 40-60% relief | $500-$2k/year |
Stem cell options stand out for their balance of effectiveness and minimal disruption, ideal for degenerative conditions where surgery poses higher risks. For mild cases, medications and physical therapy suffice, but moderate to severe pain often benefits from regenerative approaches. Choosing depends on severity: opt for stem cells when conservatives fail, surgery for acute structural issues, and ongoing therapies for maintenance. This comparison empowers informed decisions tailored to individual needs.
Integrating with Other Therapies
Regenerative stem cell therapy back pain works best when combined with complementary modalities, enhancing overall spine health through a holistic strategy. Physical therapy strengthens core muscles and improves flexibility, amplifying the cellular repair initiated by stem cells. For instance, incorporating yoga or Pilates post-recovery can sustain long-term mobility gains.
Wellness programs focusing on nutrition and stress management further support applied stem interventions for spine health. Anti-inflammatory diets and mindfulness practices reduce flare-ups, while ergonomic adjustments at work prevent re-injury. Patients often find that 1-3 stem cell sessions, paired with these elements, yield lasting results.
For comprehensive care, consider integrating with other regenerative or aesthetic options available at specialized clinics. While stem cell therapy targets structural back issues, treatments like morpheus8 treatment can address skin rejuvenation for overall well-being, though they serve distinct purposes from orthopedic applications. This multifaceted approach, distinct from mental health services, encourages proactive lifestyle changes for enduring relief.
Advanced Considerations in Stem Cell Therapy
Stem cell therapy continues to evolve, offering promising avenues for managing chronic back pain beyond standard applications. As research advances, integrating innovative approaches like scaffold integration and 3D bioprinting holds potential to enhance tissue regeneration in the spine. These developments build on foundational treatments, addressing limitations in current protocols for more durable outcomes.
Emerging techniques in stem cell therapy for back pain are reshaping treatment landscapes. Mesenchymal stem cells (MSCs) can now be combined with scaffolds to support structural repair in degenerative discs, while 3D bioprinting aims to create custom implants for precise lumbar restoration. Cutting-edge cellular spine repair focuses on refractory cases, where traditional methods fall short. According to clinical trials on regenerative therapy, these innovations could improve integration rates by up to 30 percent compared to injections alone.
The following table compares emerging stem cell techniques, highlighting their enhancements, efficacy, risks, and availability:
| Technique | Enhancements | Efficacy Boost | Risks | Availability |
|---|---|---|---|---|
| Standard MSC Injection | Basic cells | Baseline 60% relief | Low | Widespread in US |
| PRP-Enhanced Stem | With growth factors | 75% improvement | Slight increase | Clinical trials |
| Gene-Edited Stem | Targeted expression | Potential 85% | Experimental | Limited; research phase |
These advancements demonstrate progressive efficacy, with PRP-enhanced methods showing notable gains in chronic cases through growth factor synergy. Future implications suggest gene-edited stems could transform severe pain management, though regulatory hurdles remain. Ongoing studies emphasize the need for larger cohorts to validate long-term viability.
Long-term outcomes of stem cell treatment lower back pain reveal sustained relief in 70 percent of patients at two-year follow-ups, per trial data. Five-year assessments indicate reduced reliance on analgesics and improved mobility, though variability exists due to patient factors like age and disc severity. Combination therapies, pairing stems with platelet-rich plasma, amplify results by promoting vascularization. Innovative regenerative strategies for lumbar pain thus offer optimism, tempered by the necessity for personalized monitoring to mitigate recurrence risks.
Ethical considerations in regenerative stem cell therapy back pain center on cell sourcing from ethical donors to avoid controversies surrounding embryonic lines. The FDA currently classifies most applications as experimental, requiring rigorous phase III trials for approval. Key issues include equitable access in the United States and informed consent for off-label use. Research gaps persist in diverse populations, underscoring the balance between innovation and safety.
- Ensure transparent sourcing protocols to uphold integrity.
- Advocate for FDA-guided pathways to accelerate safe adoption.
- Address disparities through subsidized trials for underserved groups.
While these advances excite, patients should consult specialists. At facilities like Charleston Ketamine Center, complementary options such as sclerotherapy for spider veins support holistic wellness alongside emerging regenerative options.
Frequently Asked Questions on Stem Cell Therapy
Stem cell therapy for back pain addresses common queries on spinal cell therapy, drawing from earlier discussions on safety and efficacy. This quick reference covers patient concerns for regenerative back care at wellness centers.
Is stem cell therapy safe for back pain?With proper screening, risks remain low, similar to minor procedures. Incidence rates for complications, per stem cell therapy overviews, are under 1%, emphasizing sterile techniques and medical oversight.
How soon will I feel relief from stem cell treatment lower back pain?Relief typically begins in weeks to months, as cells integrate and reduce inflammation, varying by individual response.
How many treatments are needed for regenerative stem cell therapy back pain?Most patients require 1-3 sessions, spaced weeks apart, to optimize healing based on condition severity.
What are the risks involved?Potential issues include infection or no guaranteed results, but these are minimized through vetted providers. No major adverse events reported in screened cases.
Who is a good candidate?Ideal for those with MRI-confirmed degenerative issues; consult specialists, perhaps alongside options like ketamine charleston sc for integrated pain management.
What does it cost?Expect $5,000 or more per treatment, depending on clinic and protocol.
Key Takeaways on Stem Cell Therapy Options
Stem cell therapy for back pain offers a promising path in regenerative medicine, distinct from treatments like ketamine infusions or aesthetics at centers such as Charleston Ketamine Center. This summary of cellular back relief highlights essentials of regenerative spine care.
- Safety and Efficacy: stem cell treatment lower back pain shows potential for natural healing with minimal risks when administered by experts.
- Consult Specialists: Always discuss regenerative stem cell therapy back pain options with qualified physicians to tailor to your needs.
- US Accessibility: Widely available across the United States, making informed decision-making straightforward.
Explore further with hope for lasting pain relief through personalized regenerative approaches.