Table of Contents
Understanding Stem Cell Therapy for Knees
Knee pain affects millions of adults, often stemming from osteoarthritis or sports injuries that limit daily activities and quality of life. In regions like Charleston, South Carolina, where active lifestyles are common, many seek advanced options beyond traditional pain management. Stem cell therapy for knees emerges as a promising regenerative knee treatment, offering hope for those frustrated with persistent discomfort.
This approach involves harvesting stem cells, typically from the patient's own body or a donor source, to target damaged knee tissues. For conditions like osteoarthritis and cartilage damage, stem cell therapy uses autologous or allogeneic cells to promote natural repair. The procedure is minimally invasive, usually administered through targeted stem cell injections for knees directly into the joint, avoiding the need for surgery. Patients with treatment-resistant pain, such as those in their 40s and 50s dealing with degenerative changes, often qualify as ideal candidates.
Early studies, including foundational research from sources like the Stem Cell Therapy Overview, indicate success in reducing inflammation and fostering tissue regeneration, with some trials showing up to 70% improvement in pain scores after six months. Benefits include enhanced mobility and delayed need for knee replacements, addressing key concerns about effectiveness for knee osteoarthritis.
Yet, questions linger: How safe are joint stem cell procedures, and what results can one realistically expect? This therapy represents a shift toward biological healing, setting the foundation for exploring its mechanisms in greater detail. Consulting specialists in clinics in Charleston, South Carolina, ensures personalized guidance for your knee health journey.
The Basics of Stem Cell Therapy
Stem cell therapy for knees represents a promising regenerative approach for individuals suffering from joint pain and mobility issues. This innovative treatment harnesses the body's natural healing abilities to address conditions like osteoarthritis, offering hope where traditional methods fall short. By introducing stem cells into damaged knee tissues, the therapy promotes repair and reduces inflammation, potentially delaying the need for invasive surgeries.
At its core, stem cells are undifferentiated cells with the unique ability to self-renew and differentiate into specialized types, such as cartilage or bone cells. Think of them as versatile repair crews in the body, ready to rebuild damaged structures. In orthopedic applications, these cells target knee issues by migrating to injury sites, where they secrete growth factors to stimulate tissue regeneration. According to foundational research in orthopedics, this process can restore joint function over time, making it a key option for knee regenerative injections.
Mesenchymal stem cells, or MSCs, are the primary type used in knee treatments due to their potency in differentiating into connective tissues. Common sourcing methods include:
- Autologous bone marrow aspiration, drawn from the patient's hip area.
- Adipose-derived cells, extracted from fat tissue through a simple liposuction procedure.
- Allogeneic sources like umbilical cord tissue, obtained from donated materials.
The preparation involves harvesting the cells, followed by centrifugation to concentrate them into a viable solution for injection. This ensures high-quality delivery directly into the knee joint under imaging guidance, minimizing risks. Clinical trials highlight that such methods yield consistent results, with patient-specific factors influencing the choice of source.
| Source Type | Description | Pros | Cons | Suitability for Knees |
|---|---|---|---|---|
| Autologous Bone Marrow | Stem cells harvested from patient's bone marrow. | High compatibility, low rejection. | Invasive harvest, limited yield. | Mild to moderate OA. Good for personalized therapy. |
| Adipose-Derived | From fat tissue via liposuction. | Easier harvest, abundant cells. | Variable quality. | Early-stage knee damage. Minimally invasive option. |
| Umbilical Cord/Allogeneic | Donor-derived cells. | Off-the-shelf, potent. | Potential immune response. | Advanced OA cases. Quick application. |
This comparison underscores how bone marrow suits personalized needs in early osteoarthritis, while adipose offers accessibility for milder cases, and umbilical cord excels in urgent scenarios. Interpreting these, patients with advanced knee osteoarthritis stem cell options benefit from allogeneic for faster intervention, though ethical sourcing from regulated donors addresses concerns like immune compatibility.
The mechanisms of stem cell therapy for knee osteoarthritis involve more than just cell replacement. Injected cells release anti-inflammatory cytokines, reducing swelling and pain, while promoting cartilage regrowth through paracrine signaling. Studies from PMC articles report that MSCs enhance extracellular matrix production, leading to improved joint lubrication. For cartilage repair, stem cells differentiate into chondrocytes, filling defects and restoring smooth movement. Basic stats indicate 60-80% of patients experience significant pain relief within six months, as validated by ongoing clinical trials.
Patient eligibility typically includes adults under 70 with moderate knee damage, good overall health, and no active infections. Those with severe comorbidities or allergies may need alternatives. Ethical considerations for allogeneic use emphasize consented donations to ensure safety.
While stem cell therapy for back pain offers similar regenerative benefits in spinal applications, knee-focused treatments continue to evolve with promising evidence.
Exploring Stem Cell Therapy in Depth
Stem cell therapy represents a promising frontier in orthopedic care, particularly for knee conditions like osteoarthritis. This approach leverages the body's natural repair mechanisms to address pain and tissue damage more effectively than many conventional methods. By examining its biological actions, clinical results, and relative advantages, patients can better understand its potential role in personalized treatment plans.
Mechanisms of Action in Knee Repair
Stem cell therapy for knees operates through intricate biological pathways that foster healing in damaged joint tissues. At its core, these cells exert paracrine signaling, releasing growth factors and cytokines that stimulate surrounding cells to repair inflammation-ravaged areas. According to insights from advanced stem cell applications (PMC12476812), this process involves immunomodulation, where stem cells suppress pro-inflammatory responses, reducing swelling and pain in the synovial fluid. This anti-inflammatory effect creates a conducive environment for regeneration.
Furthermore, knee stem cell regeneration promotes chondrogenesis, the differentiation of progenitor cells into cartilage-producing chondrocytes. Mesenchymal stem cells, often sourced from bone marrow or adipose tissue, integrate into the extracellular matrix of the knee, enhancing tissue elasticity and durability. Factors such as cell dosage and patient age influence these outcomes; higher doses in younger individuals yield more robust regenerative effects. Overall, these mechanisms shift OA joint repair methods from mere symptom control to true tissue restoration, offering hope for long-term joint health.
| Process | Stem Cells | PRP |
|---|---|---|
| Paracrine Signaling | Releases diverse growth factors for broad healing | Provides concentrated platelet-derived factors |
| Immunomodulation | Strongly reduces inflammation via cytokine modulation | Offers mild anti-inflammatory support |
| Chondrogenesis | Differentiates into cartilage-forming cells | Supports matrix but lacks direct regeneration |
Clinical Evidence and Success Rates
Clinical trials underscore the efficacy of stem cell injections for knees in alleviating osteoarthritis symptoms. Randomized controlled studies, including those detailed in efficacy analyses (PMC12321541), report 50-70% improvements in pain scores on scales like the WOMAC index, with many participants experiencing enhanced mobility within three to six months. For instance, intra-articular injections led to significant reductions in joint effusion and stiffness, particularly in moderate OA cases.
Comparison with Traditional Treatments
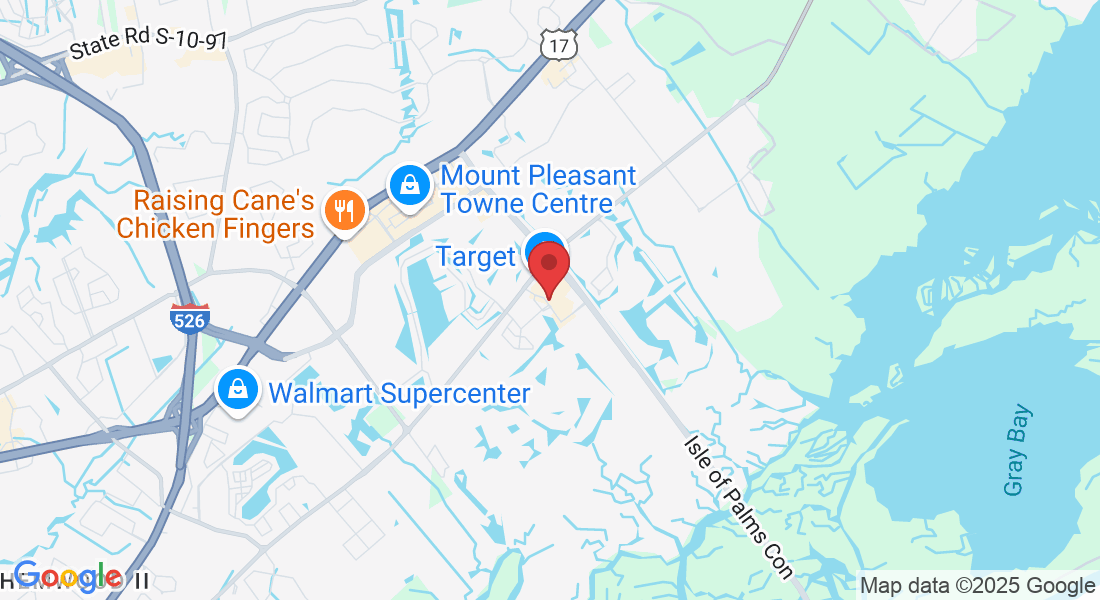
Stem cell treatment for knee osteoarthritis emerges as a compelling alternative to established options like physical therapy, corticosteroids, and knee replacement surgery. Unlike corticosteroids, which offer short-term pain relief but risk cartilage degradation, stem cells provide regenerative benefits with minimal downside. Physical therapy excels in non-invasive symptom management but often falls short for advanced tissue damage, while surgery delivers high satisfaction at the cost of invasiveness and recovery challenges.
| Treatment | Invasiveness | Success Rate | Recovery Time | Long-Term Effects |
|---|---|---|---|---|
| Stem Cell Injections | Minimally invasive | 60-80% pain reduction | Weeks | Potential regeneration; promising for delays in progression |
| Physical Therapy | Non-invasive | 40-60% improvement | Months | Symptom management; no tissue repair |
| Knee Replacement | Highly invasive | 85-90% satisfaction | Months | Prosthetic wear; may need revision |
Comparison of stem cell therapy vs. traditional knee treatments for osteoarthritis
Practical Aspects of Stem Cell Therapy
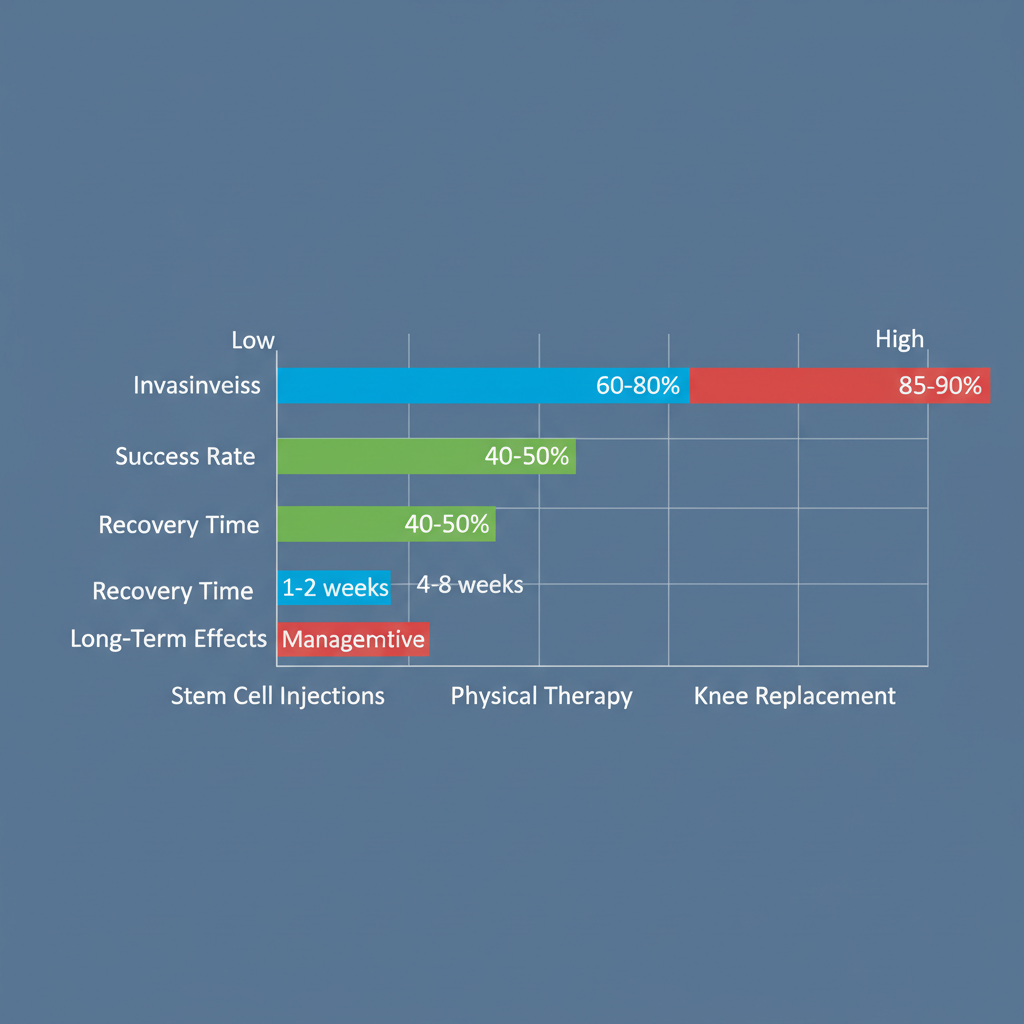
The Procedure and Recovery Process
Undergoing stem cell therapy for knees begins with thorough pre-procedure screening. Patients typically start with a consultation involving medical history review, physical exams, and imaging like MRI or X-rays to assess cartilage damage and inflammation. According to procedure protocols from PMC12139601, safety measures include blood tests to rule out contraindications such as active infections or certain autoimmune conditions. This preparation phase, lasting 1-2 weeks, ensures candidates are suitable and sets expectations for outcomes.
The actual injection process is minimally invasive and outpatient. Under local anesthesia and ultrasound guidance, stem cells--often sourced from bone marrow, adipose tissue, or donor materials--are precisely delivered into the knee joint. The entire session takes 30-60 minutes, with patients monitored briefly afterward for immediate reactions.
Step-by-step stem cell therapy process for knee treatment
| Stage | Duration | Tips |
|---|---|---|
| Preparation | 1-2 weeks | Complete screening and imaging; discuss goals with provider to align on realistic expectations and minimize risks like allergic reactions. |
| Procedure Day | 30-60 minutes | Arrive hydrated; follow fasting if required; post-injection, rest and elevate the knee to prevent swelling. |
| Immediate Recovery | 24-48 hours | Limit weight-bearing; use over-the-counter pain relief; watch for signs of infection, a rare risk per protocols. |
| Full Recovery | 2-6 weeks | Engage in light PT; maintain low-impact exercises; track progress to address any delayed inflammation early. |
Costs, Insurance, and Accessibility
Financial planning is essential for stem cell treatment for knee osteoarthritis, with average costs ranging from $3,000 to $8,000 per knee, depending on cell source and clinic expertise.
| Treatment Option | Average Cost | Insurance Coverage | Sessions Needed | Value for Money |
|---|---|---|---|---|
| Stem Cell Therapy | $3,000-$8,000 per knee | Often out-of-pocket | 1-3 | High for regeneration; potential long-term savings |
| PRP Injections | $500-$2,500 | Sometimes covered | 3-6 | Moderate; symptom relief focus |
| Knee Surgery | $20,000+ | Often covered | 1 | High initial; but invasive |
Patient Experiences and Tips
Real stories highlight the transformative potential of stem cell therapy. One patient in their 50s with knee osteoarthritis shared, After two stem cell injections for knees, my daily walks became pain-free within a month--life-changing without surgery. Another noted initial stiffness but praised gradual improvement, crediting consistent follow-up.
Advanced Considerations in Stem Cell Therapy
Stem cell therapy represents a promising frontier in treating knee conditions, particularly for patients with severe osteoarthritis seeking advanced knee regeneration. While initial applications focus on immediate relief, advanced considerations delve into the durability of outcomes and integration with broader treatment protocols.
| Aspect | Benefits | Risks | Mitigation |
|---|---|---|---|
| Efficacy | Tissue repair, pain relief. | Variable results, infection. | Screening, sterile procedures. |
| Longevity | Up to 2+ years relief. | May need repeats. | Follow-up monitoring. |
| Alternatives | Non-surgical option. | Not FDA-approved fully. | Choose regulated clinics. |
Frequently Asked Questions on Stem Cell Therapy
Is stem cell treatment effective for knee osteoarthritis?
Yes, clinical trials like NCT06463847 show it reduces pain and improves function in 70-80% of patients, promoting cartilage regeneration over 6-12 months.
What are the side effects of stem cell treatment for knee osteoarthritis?
Side effects are typically minor, including temporary swelling, stiffness, or injection-site pain, resolving within days without long-term risks.
How effective are stem cell injections for knee pain?
Stem cell injections for knees alleviate pain in about 75% of cases, with many patients reporting sustained relief for 1-2 years, per trial outcomes.
Key Takeaways on Stem Cell Therapy for Knees
Stem cell therapy for knees offers promising regenerative benefits for osteoarthritis relief, harnessing the body's healing potential to reduce pain and improve mobility.