Table of Contents
Understanding Ketamine Therapy for PTSD
Post-traumatic stress disorder (PTSD) affects about 6% of U.S. adults, manifesting in debilitating symptoms like flashbacks, hypervigilance, and emotional numbness that disrupt daily life and relationships. For those with treatment-resistant cases, ketamine therapy for PTSD emerges as a promising option, offering rapid relief where traditional antidepressants often fall short. Unlike conventional medications that may take weeks to work, ketamine targets glutamate receptors in the brain, promoting neural plasticity and synaptogenesis--essentially rewiring pathways disrupted by trauma to foster quicker mood stabilization and PTSD relief via ketamine infusions.
At clinics like the Charleston Ketamine Center, this therapeutic ketamine for trauma recovery involves supervised intravenous (IV) administrations with precision dosing tailored to individual needs. The process begins with a thorough medical screening to ensure safety, distinguishing it sharply from recreational use by emphasizing clinical oversight and integration with behavioral support. Patients in the Charleston, SC area, including Mount Pleasant, benefit from charleston ketamine therapy protocols that deliver antidepressant effects within hours, addressing core PTSD symptoms effectively.
This introduction highlights ketamine's potential as a ketamine treatment for PTSD, setting the foundation for exploring fundamentals like eligibility and protocols in subsequent sections. Understanding these basics empowers those seeking innovative paths to recovery and supports informed, confident treatment decisions.
Fundamentals of Ketamine Therapy for PTSD
Post-traumatic stress disorder affects millions, often leaving traditional treatments insufficient for rapid relief. Ketamine therapy for PTSD emerges as a promising option, particularly for those in the Charleston, SC area seeking innovative care at centers like Charleston Ketamine Center. This approach leverages ketamine's unique properties to address trauma-related symptoms more swiftly than conventional methods.
At its core, ketamine works by blocking NMDA receptors in the brain, which triggers a cascade of neurochemical changes. This antagonism promotes synaptogenesis, essentially rebuilding neural connections disrupted by trauma. Think of it as a brain reset button, fostering neuroplasticity to help patients process memories without overwhelming fear. For PTSD patients, this rapid rewiring can alleviate intrusive thoughts and hypervigilance faster than many alternatives. Clinical studies highlight ketamine's ability to enhance brain-derived neurotrophic factor, supporting long-term resilience against stress responses.
Understanding these mechanisms underscores why comparing ketamine to established treatments matters for informed decisions. Patients resistant to standard options benefit from evaluating onset, efficacy, and tolerability to tailor their path forward.
| Aspect | Ketamine Therapy | Traditional Antidepressants (SSRIs) | Cognitive Behavioral Therapy (CBT) |
|---|---|---|---|
| Onset of Relief | Hours to days | Weeks to months | Several sessions over weeks |
| Efficacy for Treatment-Resistant PTSD | High (up to 70% response rate) | Moderate (30-50% response) | Variable, often combined with meds |
| Common Side Effects | Dissociation, nausea (short-term) | Sexual dysfunction, weight gain | Emotional discomfort during sessions |
Ketamine stands out for its quick action, ideal for urgent PTSD symptom relief, though supervision mitigates transient effects like dissociation. In contrast, SSRIs build efficacy gradually but may introduce persistent issues, while CBT demands commitment over time. Data from clinical studies affirm ketamine's edge in treatment-resistant cases, making it a valuable adjunct at supervised clinics.
These comparisons highlight ketamine's role in bridging gaps left by slower therapies, yet integration with ongoing support amplifies outcomes. For visual clarity on these differences, consider the following chart that illustrates key contrasts.
Local protocols, such as those at Charleston Ketamine Center in Mount Pleasant, South Carolina, emphasize personalized dosing to maximize benefits while minimizing risks. Trauma-focused ketamine protocols typically involve an initial assessment reviewing medical history, psychiatric evaluation, and PTSD symptom severity to confirm suitability.
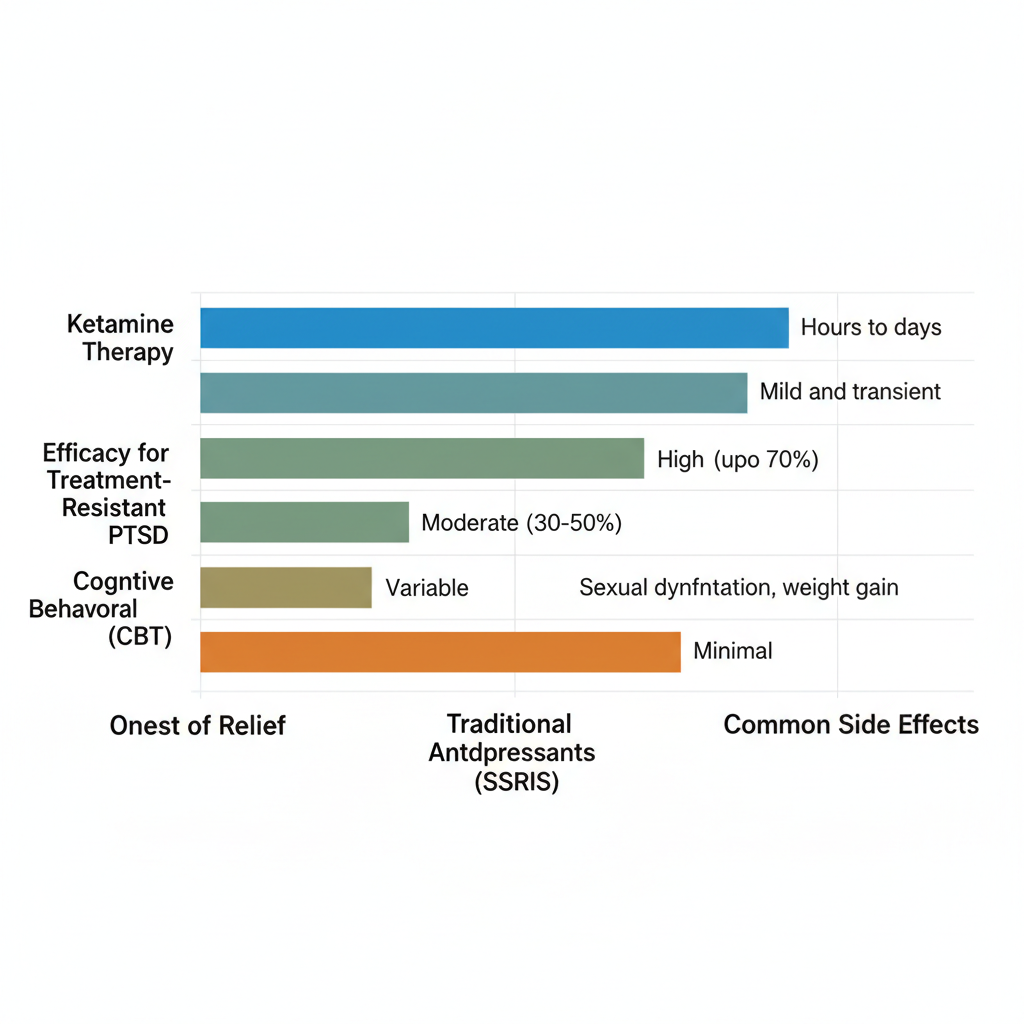
Ketamine vs traditional treatments for PTSD effectiveness comparison
Standard PTSD-targeted infusions follow a structured regimen. Patients undergo six IV sessions over two to three weeks, each lasting about 40 minutes with low-dose administration under medical monitoring. This ketamine infusion for PTSD method ensures steady delivery, promoting synaptic growth without anesthesia-level effects.
Eligibility for ketamine treatment for PTSD centers on adults with confirmed diagnosis and prior failures from SSRIs or CBT. Centers like those in Charleston, SC, exclude candidates with uncontrolled hypertension or psychosis history. Pre-treatment preparations include fasting for four to six hours beforehand to prevent nausea and arranging transportation post-session due to temporary grogginess.
For sustained gains, pairing ketamine for ptsd with talk therapy integrates insights from infusions, fostering deeper healing. Insurance coverage varies, but many clinics offer financing for accessible care in the region.
Deep Dive into Ketamine Therapy Options for PTSD
Ketamine therapy for PTSD represents a promising advancement in mental health treatment, particularly for those with treatment-resistant symptoms. At clinics like Charleston Ketamine Center in Mount Pleasant, South Carolina, this approach offers supervised care tailored to individual needs. Evidence-based PTSD ketamine protocols focus on rapid intervention, drawing from clinical guidelines to ensure safety and efficacy.
Effectiveness and Research on Ketamine Infusions
Clinical studies highlight ketamine infusion for PTSD as a breakthrough, with response rates reaching 60-70% in reducing core symptoms. A key finding from trials shows that a single infusion can lead to rapid decreases in hyperarousal, such as intrusive thoughts and heightened anxiety, often within hours. For instance, research cited in ketamine infusion therapy guidelines reports up to 70% symptom reduction in participants with combat-related PTSD, emphasizing its potential over traditional antidepressants that may take weeks to act.
These findings stem from randomized controlled trials where low-dose ketamine infusions, administered under medical supervision, targeted neural pathways disrupted by trauma. Patients experienced notable improvements in avoidance behaviors and emotional numbing, key PTSD hallmarks. Infusion-based trauma relief proves particularly effective for hyperarousal, with brain imaging studies revealing restored connectivity in fear-processing regions shortly after treatment. However, caveats include the need for maintenance sessions, as effects may wane without follow-up. This body of research underscores why ketamine stands out in PTSD management.
The following table outlines comparisons across delivery methods, informed by APNA guidelines and clinical trials, to illustrate IV infusion's advantages.
| Method | IV Infusion | Nasal Spray (Esketamine) | Oral Lozenge |
|---|---|---|---|
| Onset Time | Immediate (hours) | 40 minutes | 30-60 minutes |
| Efficacy for PTSD | High, supervised dosing | FDA-approved for depression, off-label PTSD | Lower bioavailability |
| Supervision Required | Yes, clinic-based | Yes, 2-hour monitoring | Home use possible |
Local clinic protocols emphasize IV for precision, allowing controlled dosing that maximizes benefits while minimizing risks in a supervised environment. This method suits PTSD patients seeking reliable outcomes, as variable absorption in other forms can lead to inconsistent results.
Benefits and Timeline for Symptom Relief
Benefits of ketamine treatment for PTSD often emerge swiftly, with many patients reporting relief within hours of their first infusion. At Charleston Ketamine Center, a series of six sessions typically sustains these gains, reducing nightmares and improving sleep quality over weeks. Studies show sustained effects for up to two weeks post-infusion, with cumulative improvements in mood and daily functioning as the protocol progresses.
Patients frequently describe a lifting of trauma's weight, enabling better engagement in therapy. For example, avoidance behaviors diminish, fostering reconnection with daily life. Timeline-wise, initial sessions target acute symptoms, while later ones build resilience against relapse. Costs for a full series average $3,000-$4,500, a worthwhile investment for those unresponsive to standard care near Mount Pleasant, South Carolina. Side effects, though transient, warrant discussion to set realistic expectations.
The table below summarizes common side effects and mitigation strategies under clinic supervision.
| Side Effect | Description | Mitigation Strategy |
|---|---|---|
| Dissociation | Temporary feeling of detachment | Monitored in clinic with support |
| Nausea | Mild gastrointestinal upset | Pre-treatment meds and hydration |
| Blood Pressure Increase | Short-term elevation | Vital signs checked throughout |
Supervised settings like those at local clinics effectively manage these, ensuring safety and enhancing overall benefits for PTSD recovery.
Comparing Ketamine Delivery Methods
IV infusions remain the preferred method for PTSD at clinics in Charleston, SC, due to their precision and immediate bioavailability compared to nasal sprays or oral lozenge options. While esketamine nasal spray offers FDA approval for depression and off-label PTSD use, it requires extended monitoring and may not deliver the same depth of relief for trauma-specific symptoms. Oral options, though convenient for home use, suffer from lower absorption rates, potentially reducing efficacy.
For patients seeking ketamine treatment for ptsd near me, IV stands out for its clinic-based oversight, ideal for complex PTSD cases. This approach aligns with evidence showing superior symptom control.
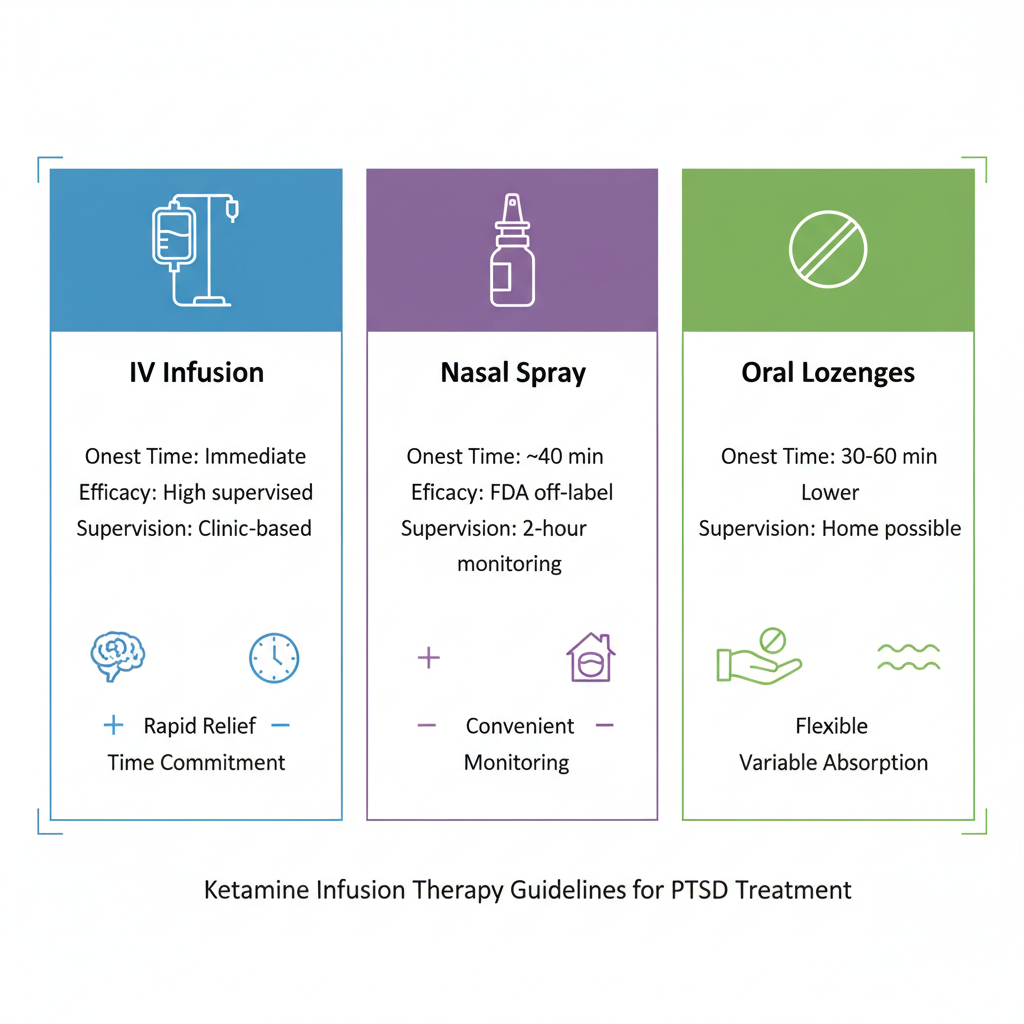
Comparison of ketamine delivery options for PTSD therapy
This visual reinforces why supervised IV protocols often yield the best results, bridging research to practical application in trauma care.
Practical Guide to Starting Ketamine Therapy for PTSD
Embarking on ketamine therapy for PTSD can mark a significant step toward relief for those with treatment-resistant symptoms. This practical guide focuses on actionable steps tailored to the Charleston area, particularly services at the charleston ketamine center in Mount Pleasant, South Carolina. Drawing from APA guidelines, which recommend exploring innovative options like ketamine after standard therapies such as cognitive behavioral therapy prove insufficient, this section outlines qualification, logistics, costs, and care management to empower informed decisions.
Finding and Qualifying for Local Treatment
Locating accessible ketamine care for trauma begins with targeted research into clinics in Charleston, SC, that specialize in mental health infusions. Start by searching for providers offering ketamine therapy for PTSD, emphasizing those with expertise in post-traumatic stress disorder protocols. The charleston ketamine center, located near Mount Pleasant, South Carolina, stands out for its outpatient focus on adults facing PTSD and related conditions.
- Contact local clinics: Reach out via phone or online forms to schedule a free initial consultation, a common offering that allows discussion of your PTSD history without commitment.
- Complete intake forms: Provide details on symptoms, prior treatments, and medical background to facilitate preliminary assessment.
- Undergo medical screening: Expect evaluation for eligibility, including checks for contraindications like uncontrolled hypertension or certain psychiatric comorbidities, ensuring safety under licensed supervision.
This process matters because proper qualification aligns practical PTSD infusion steps with evidence-based standards, reducing risks and enhancing outcomes. According to APA guidelines, sequencing ketamine after traditional interventions maximizes benefits for trauma survivors. Tips include gathering medical records in advance and preparing questions about personalization to streamline your path to starting treatment. (198 words)
Session Logistics and Costs in Charleston
Once qualified, understanding ketamine infusion for PTSD logistics ensures smooth integration into your routine. Clinics in the Charleston, SC, area, such as those near Mount Pleasant, South Carolina, typically structure treatment as a series of supervised intravenous sessions to promote neural plasticity and symptom relief.
- Schedule infusions: Book a full 6-session series spaced over 4-6 weeks, with each appointment lasting about 45 minutes plus observation time.
- Prepare for visits: Arrive hydrated and fasted lightly; a comfortable waiting area and medical monitoring await during the procedure.
- Expect the process: The IV delivers precise dosing while you relax in a calm setting, often with optional music or guided imagery for comfort.
These steps are crucial for consistent progress, as staggered scheduling allows the brain to adapt gradually. Why it matters: Structured protocols support sustained PTSD reduction beyond initial sessions. For affordability context in the region, costs vary by package, reflecting the specialized nature of ketamine treatment for PTSD.
| Session Type | Initial Consultation | Single IV Infusion | Full 6-Session Series |
|---|---|---|---|
| Average Cost (Charleston, SC) | $0 (free at many clinics) | $400-600 | $2,000-3,500 |
| Insurance Coverage | Often not covered | Rarely, case-by-case | Out-of-pocket typical |
| Duration | 30-60 minutes | 45 minutes | Over 4-6 weeks |
Based on regional clinic data; consult Charleston Ketamine Center for exact quotes. Reference APA guidelines for treatment planning.
Post-table, consider payment options like bundled discounts or financing plans offered by local providers to make ketamine treatment for PTSD more accessible. Inquire about these during consultation to align with your budget. (182 words)
Managing Side Effects and Follow-Up Care
Preparation enhances comfort during ketamine infusions, minimizing disruptions to daily life. Common reactions include temporary dissociation, nausea, or mild blood pressure elevation, typically resolving within hours under supervision.
Patient prep checklist:
- Eat a light meal 2-3 hours before; avoid heavy foods.
- Arrange safe transportation, as effects may linger briefly.
- Inform staff of any anxieties for tailored support.
These tips matter because proactive management fosters trust in the process, allowing focus on healing. Why: Side effects, while manageable, underscore the need for professional oversight per APA recommendations.
For practical value, here's a mitigation table:
| Side Effect | Mitigation Strategy |
|---|---|
| Dissociation | Pre-session relaxation techniques; post-infusion rest |
| Nausea | Anti-nausea meds if needed; ginger tea after |
| Blood Pressure Rise | Baseline monitoring; hydration emphasis |
Follow-up care integrates sessions with ongoing therapy, such as weekly check-ins or journaling progress. Monitor mood shifts and report to your provider; combining with talk therapy amplifies benefits for trauma recovery. This holistic approach ensures lasting PTSD relief. (148 words)
Advanced Considerations in Ketamine Therapy for PTSD
When evaluating advanced PTSD ketamine strategies, provider qualifications stand as a cornerstone of safe and effective care. Board-certified psychiatrists or anesthesiologists typically oversee ketamine infusions, ensuring precise dosing and monitoring for adverse effects. These experts must possess specialized training in psychiatric applications, often including certification from bodies like the American Psychiatric Nurses Association. For instance, in treatment-resistant cases, such oversight prevents complications and maximizes therapeutic benefits. Patients seeking ketamine therapy for PTSD should verify credentials through state licensing boards to confirm expertise in managing dissociative states during sessions.
Regulatory status further shapes the landscape of ketamine treatment for PTSD. While the FDA approves ketamine for anesthesia and esketamine for treatment-resistant depression, its use for PTSD remains off-label, requiring informed consent and adherence to clinical guidelines. Integration with therapies like cognitive behavioral therapy or eye movement desensitization and reprocessing enhances outcomes, as ketamine's rapid neuroplasticity effects complement traditional trauma processing. Research from sources like the American Psychiatric Association highlights how combining modalities addresses both acute symptoms and underlying neural pathways, though ongoing studies underscore the need for standardized protocols.
The following table compares ketamine against established PTSD treatments, illustrating key differences in efficacy and application:
| Factor | Ketamine Therapy | EMDR Therapy | Prolonged Exposure |
|---|---|---|---|
| FDA Approval for PTSD | Off-label | Not specifically | Evidence-based but not FDA |
| Long-Term Efficacy | Requires maintenance; promotes plasticity | High for trauma processing | Effective but exposure-intensive |
| Provider Qualifications | MD supervision, psychiatric expertise | Trained therapists | Licensed psychologists |
This comparison, drawn from APA and APNA resources, emphasizes supervised protocols at specialized centers. Integrated care proves essential, as no single approach suits all patients; blending ketamine infusion for PTSD with talk therapies fosters sustained remission while mitigating relapse risks.
Long-term management demands strategic maintenance dosing, often spaced every few weeks to sustain synaptic growth observed in neuroimaging studies. Ethical considerations include equitable access for underserved populations and avoiding over-reliance on infusions without behavioral support. Key points include:
- Prioritizing patient autonomy in consent processes.
- Monitoring for dependency in chronic use.
- Collaborating with multidisciplinary teams for holistic recovery.
At centers like those offering ketamine charleston sc, expert-supervised trauma infusions in Charleston, SC, exemplify these principles, providing tailored plans that integrate local resources for enduring PTSD relief. While promising, emerging evidence calls for cautious optimism as research evolves.
Frequently Asked Questions About Ketamine for PTSD
Will insurance cover ketamine therapy for PTSD? Ketamine remains experimental for PTSD, limiting coverage by most plans. Patients often pay out-of-pocket, though some clinics offer financing options in Charleston, SC. Consult your provider for specifics.
How many ketamine infusions are needed for PTSD relief? Typically, 4-6 infusions over weeks provide noticeable benefits in ketamine treatment for PTSD. Individual responses vary, with maintenance sessions possible for sustained effects.
Is ketamine FDA approved for PTSD treatment? No, ketamine is FDA-approved for anesthesia but used off-label for PTSD. Clinical evidence supports its efficacy, but it's not yet standard for this condition.
What are the side effects of ketamine infusion for PTSD? Common mild effects include dizziness, nausea, or elevated blood pressure, lasting 30-60 minutes post-infusion. These resolve quickly under supervision.
How quickly does ketamine therapy for PTSD work? Many experience rapid relief after 1-2 sessions, unlike traditional antidepressants. One patient reported reduced flashbacks within days at a local clinic.
Where can I access iv therapy charleston sc for PTSD? iv therapy charleston sc options are available at specialized centers near Mount Pleasant, South Carolina. Schedule a consultation for personalized care.
What alternatives exist before trying ketamine for PTSD? SSRIs or therapy like CBT are first-line options. Ketamine suits treatment-resistant cases after exhausting these approaches.
How effective is ketamine for common trauma infusion questions? Studies show 60-70% response rates. Always discuss with professionals for tailored FAQ on PTSD ketamine care.
Next Steps Toward PTSD Relief with Ketamine
In final thoughts on trauma infusions, ketamine therapy for PTSD stands out for its rapid effects. Supervised ketamine infusions for PTSD deliver quick symptom relief, often within hours, while precision dosing ensures safety and efficacy in clinical settings. This approach promotes neural plasticity, helping rebuild pathways disrupted by trauma.
The path to PTSD recovery via ketamine offers advantages beyond traditional treatments, especially when standard options fail. At Charleston Ketamine Center in Mount Pleasant, South Carolina, our expertise in ketamine treatment for PTSD combines mental health support with integrated aesthetics for holistic wellness. Local accessibility makes personalized care straightforward.
Ready to reclaim your life? Schedule a free assessment today for relief in Charleston, SC. Contact us at (843) 324-6726 or coastalketaminechs@gmail.com to begin your journey.